Isolated middle cerebral artery (MCA) dissection is a rare but serious cause of acute ischemic stroke in children. In most cases, the etiology is traumatic or idiopathic. Childhood primary angiitis of the central nervous system (cPACNS) is also a rare condition and only recently has been recognized as a potentially fatal cause of childhood stroke.1 Childhood PACNS is categorized into two subtypes: angiography-negative small vessel cPACNS, and angiography-positive large vessel cPACNS. Angiography-positive large vessel cPACNS is further divided into progressive and nonprogressive disease. Although there are no universal management guidelines for cPACNS, treatment usually consists of a combination of immunosuppressive and antithrombotic agents to prevent disease progression and complications.2 Herein we report a case in which cPACNS presented with unilateral dissection of the right MCA and multiple stenoses of the right posterior cerebral artery (PCA).
CASE
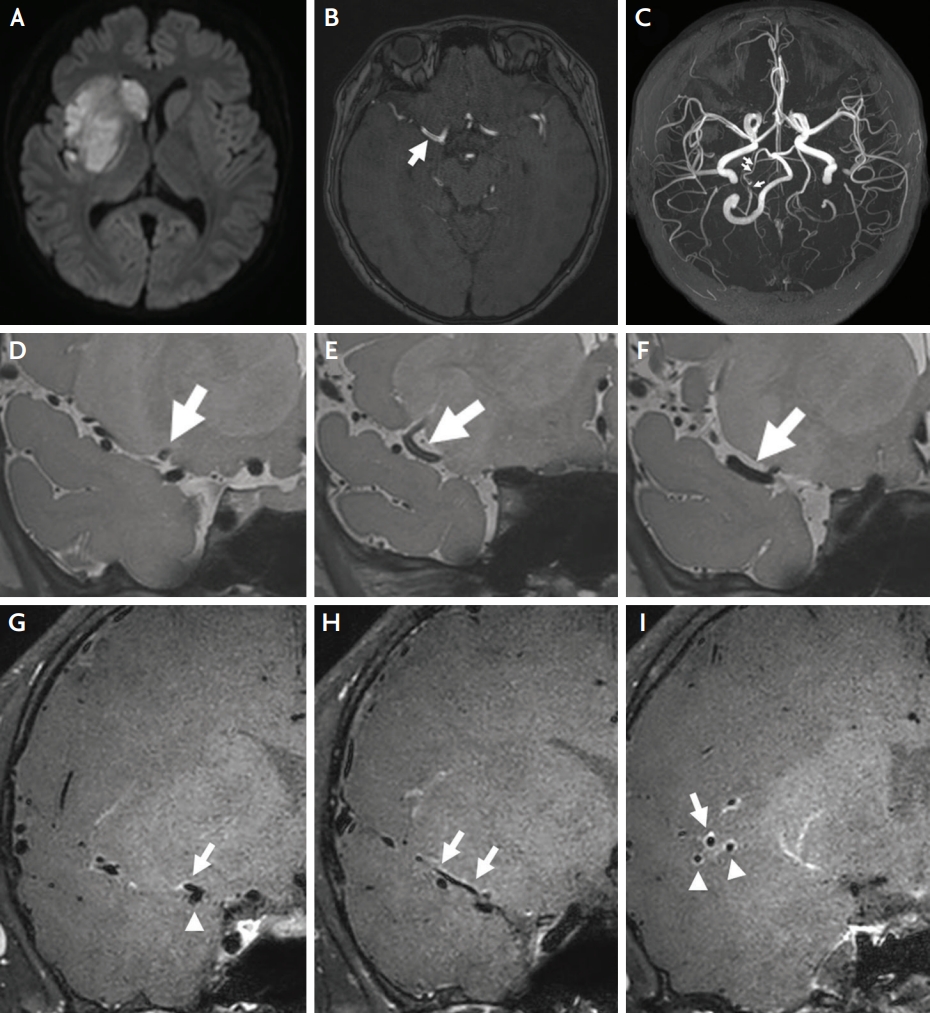
A 14-year-old healthy male with no significant previous medical history presented with acute sudden onset left-sided hemiparesis after a paroxysmal but severe headache during defecation. Recent history of trauma to the head and neck was denied. Initial neurological examination revealed left hemi-hypoesthesia whilst signs of extinction, anosognosia, and asomatognosia were not found. The initial National Institute of Health Stroke Scale score was 11 (facial palsy 2; left arm 4; left leg 4; sensory 1). He had no systemic symptoms, including fever, recent weight change, skin rash, arthritis, and dyspnea. Brain magnetic resonance imaging (MRI) was performed and showed acute right MCA infarction with a diffuse double-lumen sign at the right M1 (Fig. 1A, B).
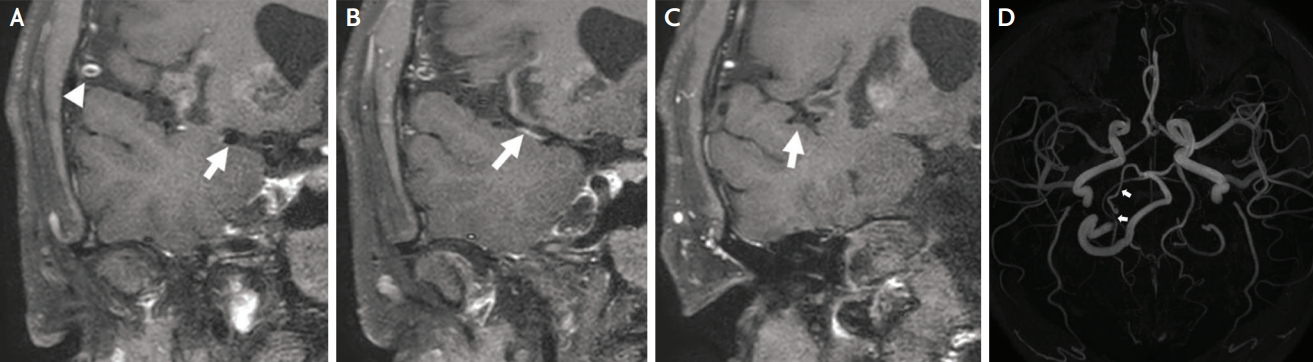
Further workup via high-resolution intracranial vessel wall imaging showed early bifurcation of the right MCA at the proximal M1 segment. Arterial dissection was noted only at the superior division on proton density imaging. (Fig. 1D-F). There was arterial wall enhancement not only at the superior division but also at the M2 segment of the inferior division (Fig. 1G-I). Diffuse narrowing of the right PCA with multiple stenosis was also seen (Fig. 1C). The multiple intracranial lesions were unexplainable with only isolated arterial dissection and were therefore considered suggestive of angiitis. Family history was negative for rheumatologic or cerebrovascular disease. On cerebrospinal fluid (CSF) examination, CSF color was slightly yellowish, opening pressure was 2 cm H2O, white blood cell count was 4/mm3, red blood cell count was 600/mm3, and protein was 36.0 mg/dL. Infection workup and cytology testing of the CSF were negative. Serum inflammatory markers including ESR (3 mm/hour) and CRP (0.05 mg/dL) were within normal limits. Other than serum antinuclear antibodies (1:80), no laboratory evidence of antibody-mediated disorders was found. Therapy with high-dose intravenous methylprednisolone (1,000 mg per day for 5 days, switched to prednisolone 60 mg on day 6) and dual antiplatelet therapy was started, and the patient was transferred to another hospital for rehabilitation. 4 months later follow up brain MRI showed improved right M1 stenosis and contrast enhancement, but narrowing and focal stenosis of the right PCA persisted (Fig. 2). His 1-year functional status as assessed on the modified Rankin scale was 3.
DISCUSSION
MCA dissection in children is rare. Nevertheless, physicians should consider intracranial artery dissection in the differential diagnosis of ischemic stroke in children. Concerning the etiology of dissection, although the prevalence of traumatic or idiopathic dissection is higher, the possibility of cPACNS should also be considered. When cPACNS is suspected, high-resolution vessel wall imaging magnetic resonance studies can be helpful. Since cPACNS is a rare and unfamiliar entity, it can be challenging to diagnose. However as untreated cPACNS is associated with high morbidity and mortality, early diagnosis and initiation of immunomodulatory therapy are of great importance.