|
 |
- Search
| J Neurosonol Neuroimag > Volume 14(1); 2022 > Article |
|
Abstract
Systemic lupus erythematosus is an uncommon cause of ischemic stroke. The subcortical and periventricular white matter are most commonly involved in the central nervous system. Although vasculitis is the most frequently mentioned etiology of stroke, it has been mainly documented in the vicinity of small-diameter vessels. In the present case, we report a young women with lupus nephritis who presented with stroke caused by large-vessel vasculitis, which was confirmed by vessel wall magnetic resonance imaging.
Systemic lupus erythematosus (SLE) is a chronic systemic autoimmune disease that affects several organs including the brain. Approximately 3-20% of SLE patients experience stroke and 15% of deaths can be explained by stroke.1 Traditionally, vasculitis, coagulopathy, and cardiac disease have been suggested to be major causes of stroke.2 Lupus vasculitis mostly involve small vessels; medium-sized vessels can also be affected, whereas involvement of large vessels is very rare.3 In the present case, we report a SLE patient with stroke caused by large-vessel vasculitis confirmed through vessel wall magnetic resonance (MR) imaging.
An 18-year-old woman presented to Chosun University Hospital Emergency Room with complaints of right-sided weakness and numbness that occurred 2 days ago. Her medical history revealed diagnosis of SLE 2 months ago. Her immunological studies revealed that FANA, antidouble stranded DNA antibody, and anti-SjogrenŌĆÖs syndrome antigen A antibody were strongly positive, whereas rheumatoid factor, anti-phospholipid antibody, lupus anticoagulant, anti-SjogrenŌĆÖs syndrome antigen B antibody, anti-cardiolipin immunoglobulin M (IgM), anti-cardiolipin IgG, and anti-╬▓2 glycoprotein 1 antibody were negative. These results strongly suggested SLE; therefore, other autoimmune diseases, including antiphospholipid antibody syndrome and SjogrenŌĆÖs syndrome, were excluded. The patientŌĆÖs generalized edema and severe proteinuria could be explained by SLE.
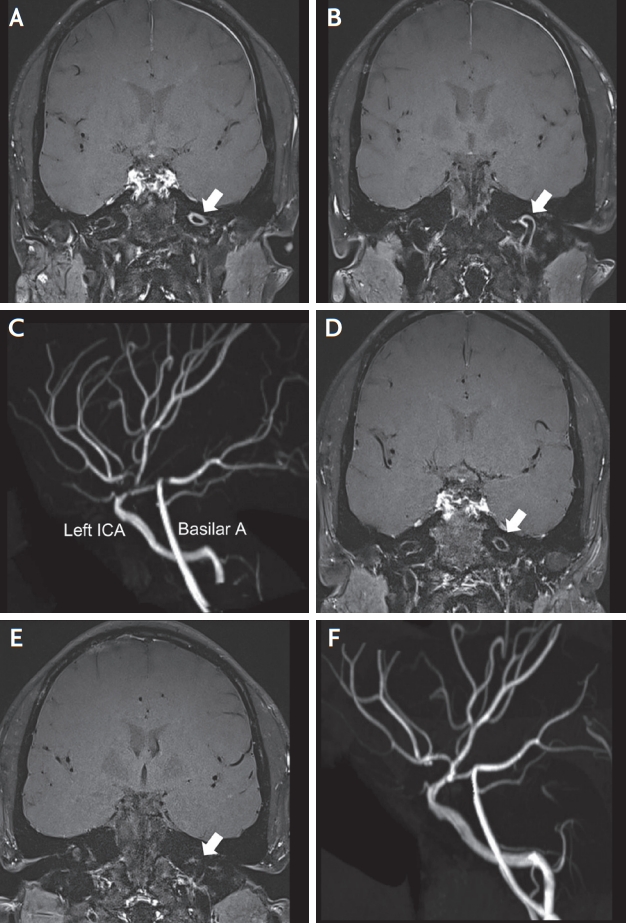
After treatment with prednisolone 20 mg and mycophenolate 2,000 mg, generalized edema and proteinuria gradually improved. Neurological examination revealed right hemiparesis (grade 4 of Medical Research Council) and numbness on the right side. The National Institutes of Health Stroke Scale score was 3. She had no headache. Diffusion-weighted brain MR images revealed multifocal acute infarctions in the left cerebral hemisphere, which were presumed as internal and external watershed zones (Fig. 1). Thickening and contrast enhancement of the endothelium were observed from the petrous to the distal cervical internal carotid artery (Fig. 2A, B). Brain MR angiography revealed multiple stenoses in the distal internal carotid artery, proximal segments of the posterior cerebral artery, and anterior cerebral artery (Fig. 2C). Carotid duplex sonography and electrocardiography findings were normal. Transthoracic echocardiography revealed no abnormalities. There were no suspicious findings for cardioembolic sources. Laboratory examination showed the following values: hemoglobin 9.3 g/dL, albumin 2.1 g/dL, cholesterol 462 mg/dL, triglycerides 204 mg/dL, low density lipoprotein 333 mg/dL, erythrocyte sedimentation rate 126 mm/hour and C-reactive protein 0.95 mg/dL. On urinalysis, protein excretion revealed four positives. In addition to prednisolone and mycophenolate, clopidogrel (75 mg) and atorvastatin (40 mg) were prescribed for stroke prevention.
Three months later, her neurological symptoms had completely improved. On follow-up brain MR angiography, initial stenosis and concentric wall enhancement were improved (Fig. 2D-F).
Unlike reported lupus vasculitis, which usually occurs in small vessels, territorial stroke due to cerebral arteritis, mainly involving the carotid artery was observed in our case.
Although small vessel vasculitis is very common, large vessel vasculitis has rarely been reported in SLE patients.4 Due of the difficulty of performing postmortem brain biopsy, the pathology of large-vessel vasculitis in SLE patients has not been established.5 However, the mortality rate in patients with large-vessel vasculitis is extremely high (approximately 67%). To prevent fatal outcomes, immediate diagnosis and aggressive immunosuppressive treatment are needed.6
The etiology of cerebral infarction includes large vessel atherosclerosis, cardioembolic sources, and small vessel disease. Various causes of vascular stenosis and inflammation can develop in patients with SLE. Lupus vasculitis is generally classified as a small-vessel vasculitis caused by immune complexes. Through T-cell antibody-mediated immune response and B-cell-induced autoimmune antibody response, it forms an immune complex and secretes cytokines, which cause inflammation in the blood vessels.7
TakayasuŌĆÖs arteritis was excluded as there was no evidence of endothelial thickening on carotid ultrasound and the extracranial carotid artery on vessel wall magnetic resonance angiography showed no enhancement. The possibility of antiphospholipid syndrome was excluded from the negative results for anticardiolipin IgM and anti-╬▓2 glycoprotein 1 antibody. Among diseases showing intracranial vascular stenosis, reversible cerebral vasospasm syndrome (RCVS) and Moyamoya disease do not require anti-inflammatory or immunosuppressive treatments, so it is important to exclude them. The patient had no symptoms such as headache. RCVS brain imaging findings showed multifocal stenosis. So, RCVS could be excluded with concentric contrast enhancement. Moyamoya disease was also considered unlikely.8
The recent development of imaging technology allows immune vasculitis diagnosis that shows increased enhancements of irregular vessel walls along the intracranial arteries.9 CNS vasculitis typically shows smooth, homogeneous, and concentric vessel wall thickening on MR imaging. It is different from atherosclerotic plaque images, which are more proximal and show eccentric and irregular vessel wall abnormalities in the intracranial arteries. However, since clinical disease activity and vessel wall MR imaging findings in intracranial artery vasculitis are not always correlated, the effect of specific treatments on vessel wall MR imaging, such as corticosteroid administration, can be observed.10 The initial thickening and concentric contrast in multiple cerebral arteries improved after 3-months of treatment. This indicates that the cause of vascular stenosis in this case was vasculitis, not a vulnerable plaque. Therefore, vessel wall imaging was useful in determining whether the patient responded to treatment. Large-vessel vasculitis should be considered a type of vasculopathy, which may be associated with serious complications such as territorial stroke. It is presumed that the latest imaging techniques, such as brain vessel wall MR imaging, can help in rapid diagnosis and increase treatment responsiveness.
NOTES
Ethics statement
This study was approved by the Institutional Review Board (IRB) of Chosun University Hospital (IRB No. 2022-01-011), and the requirement for informed consent was waived.
Fig.┬Ā1.
Diffusion weighted images of the lesion. (A, B) Multifocal acute infarcts in left cerebral hemisphere, probably internal and external watershed zone.
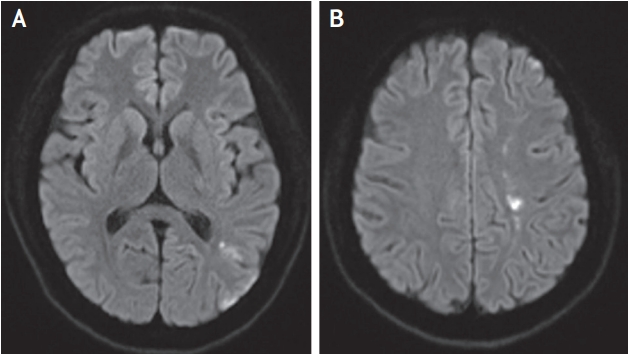
Fig.┬Ā2.
Contrast-enhanced vessel wall magnetic resonance angiography and time of flight magnetic resonance angiography. (A, B) T1 contrast-enhanced vessel wall magnetic resonance shows thickening of the vessel wall and concentric contrast enhancement from the proximal to the distal of the internal carotid artery (petrous and distal cervical ICA) (white arrows). (C) Time of flight magnetic resonance angiography shows multiple stenosis in the distal internal carotid artery, the proximal segments of posterior cerebral artery and anterior cerebral artery (white arrows). (D-F) Follow-up contrast-enhanced vessel wall magnetic resonance angiography and time of flight magnetic resonance angiography performed 3 months later shows recovery of the arterial stenosis and wall enhancement. ICA; internal carotid artery.
REFERENCES
1. Futrell N, Millikan C. Frequency, etiology, and prevention of stroke in patients with systemic lupus erythematosus. Stroke. 1989;20:583-591.


2. Nikolopoulos D, Fanouriakis A, Boumpas DT. Cerebrovascular events in systemic lupus erythematosus: diagnosis and management. Mediterr J Rheumatol. 2019;30:7-15.



3. Leone P, Prete M, Malerba E, Bray A, Susca N, Ingravallo G, et al. Lupus vasculitis: an overview. Biomedicines. 2021;9:1626.



4. Takeshita S, Ogata T, Tsugawa J, Tsuboi Y. Isolated cerebral vasculitis in the unilateral middle cerebral artery in a case with SLE. Intern Med. 2020;59:3225-3227.



5. Ide S, Kakeda S, Miyata M, Iwata S, Ohkubo N, Nakayamada S, et al. Intracranial vessel wall lesions in patients with systematic lupus erythematosus. J Magn Reson Imaging. 2018;48:1237-1246.



6. B├Čckle BC, Jara D, Aichhorn K, Junker D, Berger T, Ratzinger G, et al. Cerebral large vessel vasculitis in systemic lupus erythematosus. Lupus. 2014;23:1417-1421.



7. Conen KL, Jeanneret C, Hecker B, Cathomas G, Biedermann BC. Acute occlusive large vessel disease leading to fatal stroke in a patient with systemic lupus erythematosus: arteritis or atherosclerosis? Arthritis Rheum. 2006;54:908-913.


8. Edjlali M, Qiao Y, Boulouis G, Menjot N, Saba L, Wasserman BA, et al. Vessel wall MR imaging for the detection of intracranial inflammatory vasculopathies. Cardiovasc Diagn Ther. 2020;10:1108-1119.