Impact of Severe Cervical Foraminal Stenosis on Contralateral C7 Nerve Transfer Outcomes
Article information
Abstract
This report presents the case of a 67-year-old male patient with severe bilateral C6/7 foraminal stenoses who underwent contralateral seventh cervical nerve (C7) transfer as a treatment for left spastic hemiparesis resulting from a right middle cerebral artery infarction. The initial postoperative results showed improved spasticity and motor function, but these gains plateaued and even receded, unlike other studies that noted progress at 10–18 months post-surgery. We hypothesized that the presence of C7 radiculopathy due to severe cervical foraminal stenosis may affect long-term outcomes after contralateral C7 transfer and serve as a contraindication for this surgery. These findings emphasize the importance of thoroughly assessing patients with cervical foraminal stenosis and the associated risk of radiculopathy before considering a contralateral C7 transfer. Further research is needed to assess the prevalence of cervical foraminal stenosis in patients undergoing contralateral C7 transfer and explore alternative surgical approaches or adjunctive treatments to optimize postoperative outcomes.
Contralateral seventh cervical (C7) nerve transfer is a potential neurosurgical intervention for mitigating the long-term motor impairments following stroke.1-4 The procedure, which involves connecting the ipsilesional C7 (recipient) to the contralesional C7 (donor), was initially established to enhance motor function in the ipsilesional arm of patients with brachial plexopathy.5 Recent studies, including a randomized controlled trial, have shown its efficacy in recovering spastic arm paralysis in patients with cerebral injuries such as stroke and encephalitis.1,2 However, some conditions may limit its success. This case report describes a patient with severe cervical foraminal stenosis who underwent contralateral C7 transfer for left spastic hemiparesis following right MCA infarction. We explored the implications of this condition on the outcome of the procedure and suggest that the risk of C7 radiculopathy may be a contraindication for contralateral C7 transfer. A thorough assessment of foraminal stenosis is crucial because severe cervical foraminal stenosis can contribute to C7 radiculopathy, diminishing the benefits of the procedure.
CASE
A 67-year-old male patient presented with left spastic hemiparesis, a long-term sequela of a right middle cerebral artery infarction that occurred 22 years previously. The patient had a modified medical research council (MRC) grade of 4 for left shoulder flexion, while the remaining left arm muscles were grade 1. Ashworth Grade 4 contractures were observed in the left elbow, wrist, and finger joints. Preoperative magnetic resonance imaging of the brachial plexus revealed severe bilateral C6/7 foraminal stenoses accompanied by findings suggestive of radiculopathy in the right arm with serratus anterior muscle denervation (Fig. 1).6 The patient displayed no motor or sensory symptoms of radiculopathy in either arm, and opted for surgery.
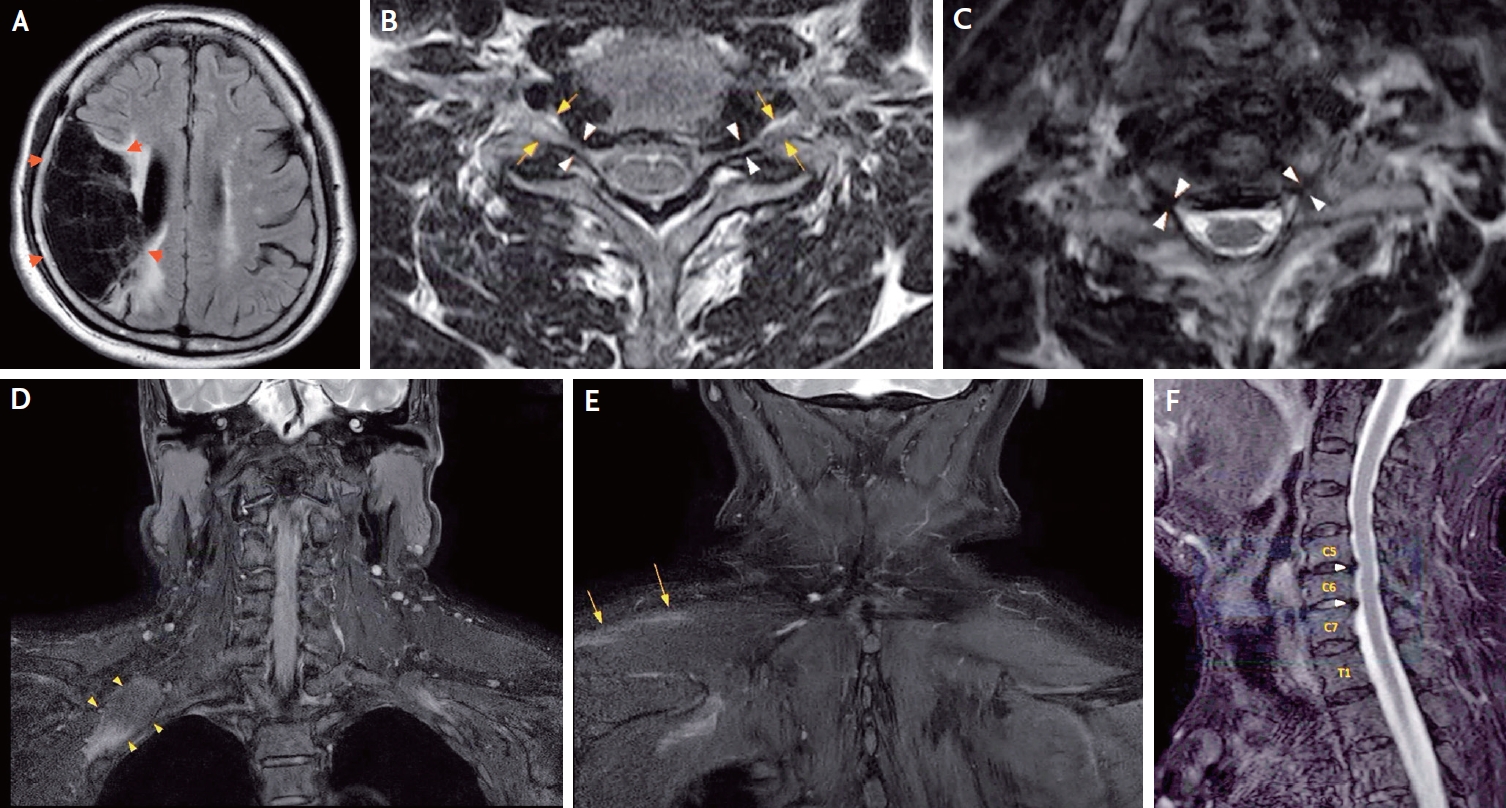
(A) Axial FLAIR sequence of the brain magnetic resonance imaging (MRI) reveals a chronic infarct with associated cerebromalacia in the right middle cerebral artery territory. (B) Cervical spinal cord MRI from 3 years before surgery displays grade 2 neural foraminal stenosis, as classified by Kim’s criteria.6 (C, F) Preoperative brachial plexus MRI demonstrates severe C6/C7 neural foraminal stenosis on the axial image (C) and mild central canal stenosis at the C5/C6 and C6/C7 levels on the sagittal image (F). (D, E) Preoperative brachial plexus MRI indicates early denervation changes in the right serratus anterior muscle (D, innervated by C5-C7 roots) and the right trapezius muscle (E, innervated by C3-C4 roots and the spinal accessory nerve).
The patient underwent a contralateral C7 transfer using the prespinal technique.1 Direct neurorrhaphy between the bilateral C7 cut ends was accomplished without tension and no significant intraoperative issues arose. Subsequently, the patient underwent rigorous rehabilitation. At each visit, the degree of motor recovery in the recipient arm was assessed using various outcome measures.
No permanent complications arose from the surgery except for immediate postoperative pain in the patient’s right hand (donor side), which gradually subsided within the first month. Both gross and fine motor functions of the recipient hand, as indicated by the dynamometer and New Jebson hand function test (NJHFT), improved in the initial months postoperatively, followed by a subsequent decline. The Fugl-Myer score and modified Barthel index displayed similar patterns, with an initial plateau or improvement during the first seven months and deterioration thereafter.
Twelve months postoperatively, the patient’s left middle and index finger extensions, as measured by the MRC grade, improved from grade 1 to grade 3, with no changes detected in the other arm muscles, with no changes detected in the other arm muscles. The patient began experiencing paresthesia in the 2nd and 3rd distal fingertips of the recipient hand at 12 months postoperatively (Fig. 2). Follow-up brain computed tomography was performed to rule out new structural lesions as the cause of neurological deterioration; all scans yielded negative results.

The upper figure demonstrates postoperative changes in Fugl-Meyer Assessment (FMA) scores of the left arm and the Modified Barthel Index (MBI). The FMA score for the left arm (max score 66; with higher scores representing enhanced functionality) plateaued at months 2 and 5, then decreased at month 7 postoperatively. MBI scores (max score 100; with higher scores reflecting better functional independence) showed progress until month 5, before declining. The lower figure highlights postoperative changes in dynamometer grip strength and the New Jebson Hand Function Test (NJHFT) after tendon transfer. The grip strength (in pounds) reached its peak at 5 months postoperatively, then deteriorated. The NJHFT (assessing the time needed to accomplish a specified task; where less time denotes better fine hand movements) exhibited progress in the initial 2 months but declined post 5 months.
DISCUSSION
In this case report, we describe a patient with severe bilateral cervical foraminal stenosis who underwent contralateral C7 transfer for the treatment of left spastic hemiparesis following a right MCA infarction. The overall recovery rate reached peaked and plateaued from 5–7 months following nerve transfer, which is contradictory and short-lived compared to previous randomized controlled trials, where most functional improvements occurred after 10 months and persisted for up to 18 months after the transfer.1
Severe cervical foraminal stenosis can lead to C7 radiculopathy, potentially attenuating the benefits of contralateral C7 transfer. Our findings indicate that the presence or risk of C7 radiculopathy may be a relative contraindication for contralateral C7 transfer. This highlights the importance of thoroughly evaluating patients with cervical foraminal stenosis and the associated risk of radiculopathy before considering this procedure.
Further research is warranted to determine the prevalence of cervical foraminal stenosis in patients undergoing contralateral C7 transfer and evaluate its impact on surgical outcomes. Additionally, future studies should explore alternative surgical approaches or adjunctive treatments for patients with severe cervical foraminal stenosis to optimize postoperative outcomes.
Notes
Ethics Statement
The requirements for approval of the Institutional Review Board and informed consent were waived due to the retrospective nature of this study.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author upon reasonable request.
Sources of Funding
None.
Conflicts of Interest
No potential conflicts of interest relevant to this article was reported.
Acknowledgements
None.
