Hemorrhagic Stroke and Blindness after Hyaluronic Acid/Polylactic Acid Filler Injection
Article information
Abstract
The number of people receiving facial filler injections is increasing as it is relatively safe than the other cosmetic procedures. However, complications of facial filler injection range from mild redness and inflammation to cerebral infarction. We report the case of a patient who was diagnosed with cerebral infarction and intracranial hemorrhage after facial filler injection. A 61-year-old male presented to the emergency department with ocular pain and visual loss in the left eye after filler injection into the glabella. Neurological examination revealed monocular blindness. Initial brain magnetic resonance imaging (MRI) revealed small, acute multifocal infarctions in the left frontal, parietal, and temporal lobes. Follow-up MRI revealed subarachnoid hemorrhages in the left frontal and parietal lobe. Follow-up brain computed tomography showed small intracerebral hemorrhage in the left frontal lobe. Clinicians must be aware that not only cerebral infarction, but intracranial hemorrhage could also be a potential adverse effect of the cosmetic filler injection in the face.
Facial filler injection is a widely accepted invasive procedure in Korean cosmetic clinics. An increase in the popularity of filler injections has led to a surge in reports regarding serious adverse effects after the procedure.1 Adverse effects after injection range from minor events such as swelling, bruising, and redness to more severe events such as cerebral infarction and visual loss. Retrograde embolic infarction has been suggested as the mechanism for cerebral infarction after injection.2-4 Although there have been several reports of cerebral infarction and visual loss following facial filler injections, spontaneous intracranial hemorrhage after filler injections has not been previously reported. Herein, we report the case of a patient who was initially diagnosed with cerebral infarction and subsequently developed intracranial hemorrhage after receiving a cosmetic filler injection into the glabella.
CASE
A 61-year-old male presented to the emergency department with sudden ocular pain and visual loss in the left eye 10 minutes after receiving a cosmetic filler injection into the glabella. The filler injection comprised of 25% hyaluronic acid and 75% poly-L-lactic acid. The patient had a history of hypertension, for which he had been taking amlodipine and candesartan. He had no history of cardiovascular disease. His initial vital signs were as follows: blood pressure, 131/70 mmHg, heart rate, 80 beats/min, respiratory rate, 20/min, and body temperature, 36.7°C. Electrocardiography revealed a sinus rhythm. Initial blood tests were within normal limits, including a complete blood cell count and routine chemistry panel. He was consciousness and his neurologic examination was normal. Physical examination at the emergency department showed redness on the left forehead, periorbital, and glabellar area. His vision was 20/20 in the right eye, but the left eye vision was limited to only light perception. Ophthalmologic examination showed sluggish pupillary light reflex and afferent pupillary defect in the left eye. Fundoscopic examination of the patient’s left eye showed segmented irregularities of retinal arterioles, edematous macula, and cherry red spot, which indicated central retinal artery occlusion (Fig. 1A).
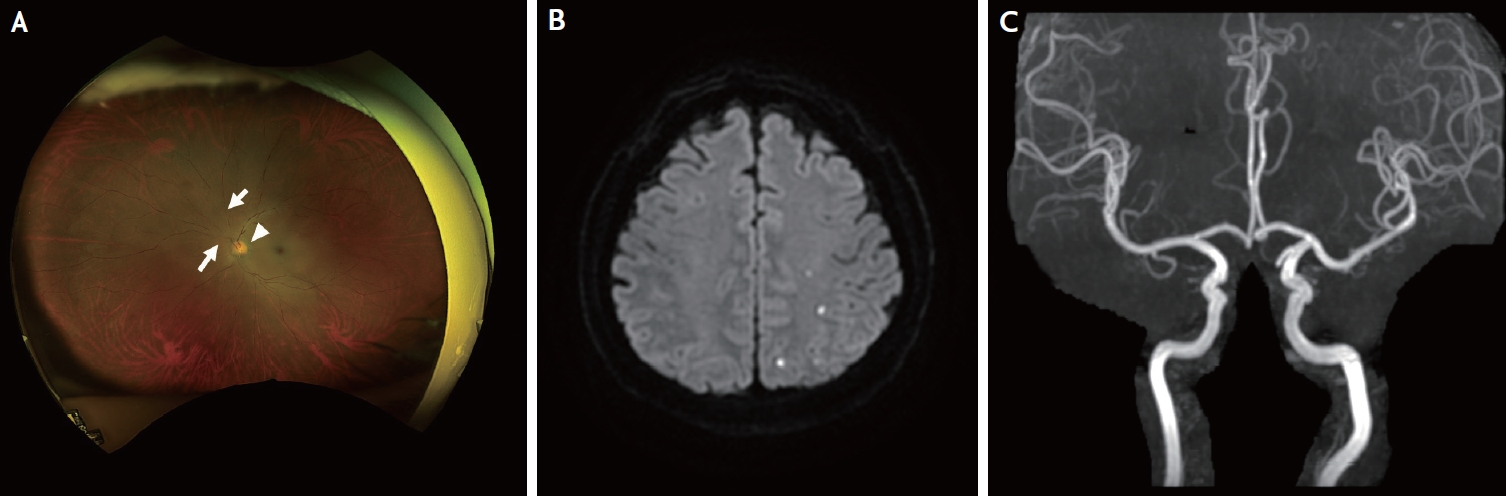
Fundoscopy, magnetic resonance imaging, and magnetic resonance angiography (MRA) findings. Initial fundoscopic examination of the patient’s left eye showing segmented irregularities of retinal arterioles (arrows), edematous macula (arrowhead), and cherry red spot (A). Initial diffusion-weighted image shows multiple scattered lesions in left frontal and parietal lobes (B). Initial MRA shows no significant stenosis in the intracranial arteries (C).
Diffusion-weighted imaging revealed small, acute multifocal infarctions in the left frontal and parietal lobes (Fig. 1B). Magnetic resonance angiography (MRA) showed no steno-occlusive lesions of the intracranial artery (Fig. 1C). To prevent further infarctions, treatment with an antiplatelet agent (aspirin 100 mg/day) was initiated. However, small subarachnoid hemorrhages were observed in the left frontal and parietal lobes on the susceptibility-weighted-imaging on the second day after admission (Fig. 2A). Consequently, the antiplatelet therapy was discontinued. On the fourth day after admission, another small intracerebral hemorrhage was found in the left frontal lobe on a follow-up brain computed tomography (Fig. 2B).

Follow-up magnetic resonance imaging and computed tomography (CT) images. Susceptibility-weighted-imaging sequence shows small subarachnoid hemorrhages in the left frontal and parietal lobes (A). Follow-up CT shows a small intracerebral hemorrhage in the left frontal lobe (B).
No other neurologic deficits were observed during admission. The pain and redness in the left forehead, periorbital, and glabellar area improved after regular wound dressings. However, the left eye vision showed no improvement. He was discharged one week after admission.
DISCUSSION
We report the unique case of combined cerebral infarction, visual loss, and intracranial hemorrhage after a facial filler injection.
Retrograde arterial emboli have been suggested as the mechanism for arterial occlusion after filler injection.2 During facial filler injection, injection material may accidentally enter the arterial system and form emboli. When injection pressure exceeds systolic arterial pressure, filler emboli can be pushed to proximal sites of the arterial system. Emboli passing through the supraorbital or supratrochlear artery can obstruct the ophthalmic artery or the central retinal artery, causing visual loss. If the emboli travel proximally further into the internal carotid artery, they can obstruct cerebral arteries by anterograde embolism.3,4
Several researchers have reported the use of an antiplatelet agent, hyperbaric oxygen, and steroids for the treatment of acute ischemic stroke after facial filler injection. However, there are currently no randomized clinical trials or treatment guidelines available.5,6 A prior animal study has suggested that intravascular hyaluronic acid emboli could induce the formation of red thrombus. In such cases, the use of intravenous urokinase and hyaluronidase can be beneficial.7 Based on this idea, the use of intravenous recombinant tissue plasminogen activator (IV-rtPA) in filler-induced acute ischemic stroke has been reported in a case report.8 The use of intravenous hyaluronidase infusion as a treatment for filler-induced acute ischemic stroke has not yet been reported.
Although there are currently no reports of spontaneous intracranial hemorrhage after filler injection, an underlying mechanism can be postulated based on previous studies. A previous in vitro study has shown that hyaluronic acid binds to human endothelial cells.9 A recent study has reported that hyaluronic acid can play a role in progress of acute ischemic hemorrhagic stroke patients through inflammatory responses.10 Since hyaluronic acid is a ligand for Toll like receptor (TLR), an increase in plasma hyaluronic acid level can trigger TLR associated immune responses. Therefore, intravascular hyaluronic acid might have caused an immune response within intracranial arteries and its endothelial cells, leading to blood-brain barrier disruption and intracranial hemorrhage. In summary, we present the case of cerebral infarction, subarachnoid hemorrhage, and intracerebral hemorrhage after filler injection. Although cerebral infarction and visual loss have been reported as possible complications after filler injection, clinicians should also recognize that intracranial hemorrhage is a potential complication after injection.
Notes
Ethics Statement
Informed consent as required by the Institutional Review Board (IRB) of Gangnam Severance Hospital was obtained from the patient.
Availability of Data and Material
The authors confirm that the data supporting the findings of this study are available within the article.
Sources of Funding
None.
Conflicts of Interest
No potential conflicts of interest relevant to this article was reported.
Acknowledgements
None.
