A Case of Klebsiella pneumoniae Meningitis Associated with Brain Abscess and Endophthalmitis
Article information
Abstract
Meningitis, brain abscess, and endophthalmitis are rare manifestations of K. pneumoniae infection. We present a case of Klebsiella meningitis associated with a brain abscess and endophthalmitis. A 58-year-old man with alcoholic liver cirrhosis and hepatocellular carcinoma presented with fever, pain in the right eyeball, and vision loss. Endophthalmitis and urinary tract infections were identified through ophthalmologic examination and urine analysis, respectively, and empirical antibiotic therapy was administered. Approximately seven days after treatment, the patient presented with persistent headaches. In the cerebrospinal fluid study, the white blood cell count was 210/mm3, the protein level was 540 mg/dL, and the glucose level was 28.6 mg/dL. Magnetic resonance imaging of the brain revealed diffuse brain abscesses in both hemispheres. Klebsiella pneumoniae was isolated from the blood and urine cultures. After intravenous injection of antibiotics (vancomycin and ceftriaxone) for 2 months, the headache resolved and the results of the cerebrospinal fluid study were normal.
Bacterial meningitis is a life-threatening infection that remains a clinical challenge, despite advancements in diagnostic methods and various antibiotic options. Among the various pathogens causing bacterial meningitis, Klebsiella pneumoniae is considered a rare pathogen. Klebsiella spp. account for less than 3% of community-acquired bacterial meningitis cases.1 However, the mortality rate in patients with Klebsiella pneumoniae infections is very high, ranging from 48.5% to 66.0% depending on reports, and Klebsiella pneumoniae accounts for 50% of severe meningitis cases in adult patients,2-4 so early detection of pathogens and appropriate and prompt treatment are critical for recovery. Klebsiella pneumoniae commonly causes sepsis, pneumonia, urinary tract infections, and liver abscesses. However, meningitis, brain abscess, and endophthalmitis are rare manifestations of K. pneumoniae infection.
Here, we report a case of Klebsiella meningitis associated with brain abscess and endophthalmitis. The patient presented with fever, headache, right eyeball pain, and vision loss, which were relieved after receiving appropriate treatment.
CASE
A 58-year-old man presented with fever, right eyeball pain, and vision loss that had lasted for two days prior to admission. Previously, the patient had shown signs of chronic alcoholism and a history of alcoholic liver cirrhosis and hepatocellular carcinoma. At the time of admission, his vital signs included body temperature of 39.3°C, heart rate of 126 beats/min, blood pressure of 92/64 mmHg, respiratory rate of 32 breaths/min, and oxygen saturation of 99% on room air. Neck stiffness, motor weakness, and cognitive decline were observed on neurological examination. Brain computed tomography (CT) revealed no abnormalities. A chest radiograph did not show any abnormal findings, and electrocardiography revealed a sinus rhythm.
The patient’s white blood cell count was 12,470/μL, with an elevated neutrophil percentage of 90.2%, platelet count of 53,000/μL, C-reactive protein level of 18.9 mg/dL, and erythrocyte sedimentation rate of 64 mm/h. Urine analysis revealed 10–29 pus cells per high-power field. An ultrasound scan of his abdomen did not reveal any liver abscess. Ophthalmoscopy and sonographic examination revealed a hazy fundus due to severe vitritis and increased echogenicity in the right eyeball (Fig. 1). The patient was initially diagnosed with a urinary tract infection (primary focus), endophthalmitis, and sepsis, and treatment with intravenous empirical antibiotic therapy (ceftriaxone) was immediately initiated and lasted for one week.
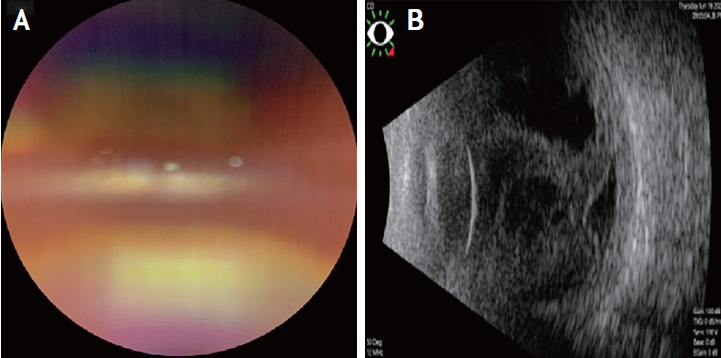
Anterior photographs of the right eye. (A) Fundus photograph revealing hazy fundus due to severe vitritis. (B) Sonogram showing increased echogenicity in the right eyeball.
On the seventh day after admission, he complained of persistent headache, and the visual analog scale score ranged from 7 to 9 points for pain on both sides of the head. On neurological examination, neck stiffness was observed. A cerebrospinal fluid (CSF) study showed that the intracranial pressure was 250 mmH2O, white blood cell count was 210/mm3 with a neutrophil percentage of 72%, lymphocyte percentage of 20%, monocyte percentage of 8%, protein level of 540 mg/dL, and glucose level of 28.6 mg/dL. Antibiotic therapy (vancomycin 1 g and ceftriaxone 2 g every 12 hours) was administered to treat bacterial meningitis. Brain magnetic resonance imaging (MRI) revealed multiple scattered ring-enhancing lesions on contrast-enhanced T1-weighted imaging and T2-fluid attenuated inversion recovery images with hyperintense lesions on diffusion-weighted images in the right frontal cortex and subcortex, left frontal, parietal, temporal, insular cortex, and basal ganglia, with meningeal enhancement in the left medial frontal sulci (Fig. 2A-F). We initially considered multiple brain abscesses with meningitis or brain metastasis of the cancer. All CSF cultures, viral PCR, and CSF cytology were negative. There was no evidence of primary cancer or primary focus of infection on chest or abdominal CT. Klebsiella pneumoniae was isolated from the blood and urine cultures. After intravenous injection of antibiotics (vancomycin and ceftriaxone) for 2 months, the fever, headache, and right eyeball pain resolved, and the results of the cerebrospinal fluid study were normal. Follow-up diffusion-weighted imaging revealed resolved hyperintense lesions (Fig. 2G, H).
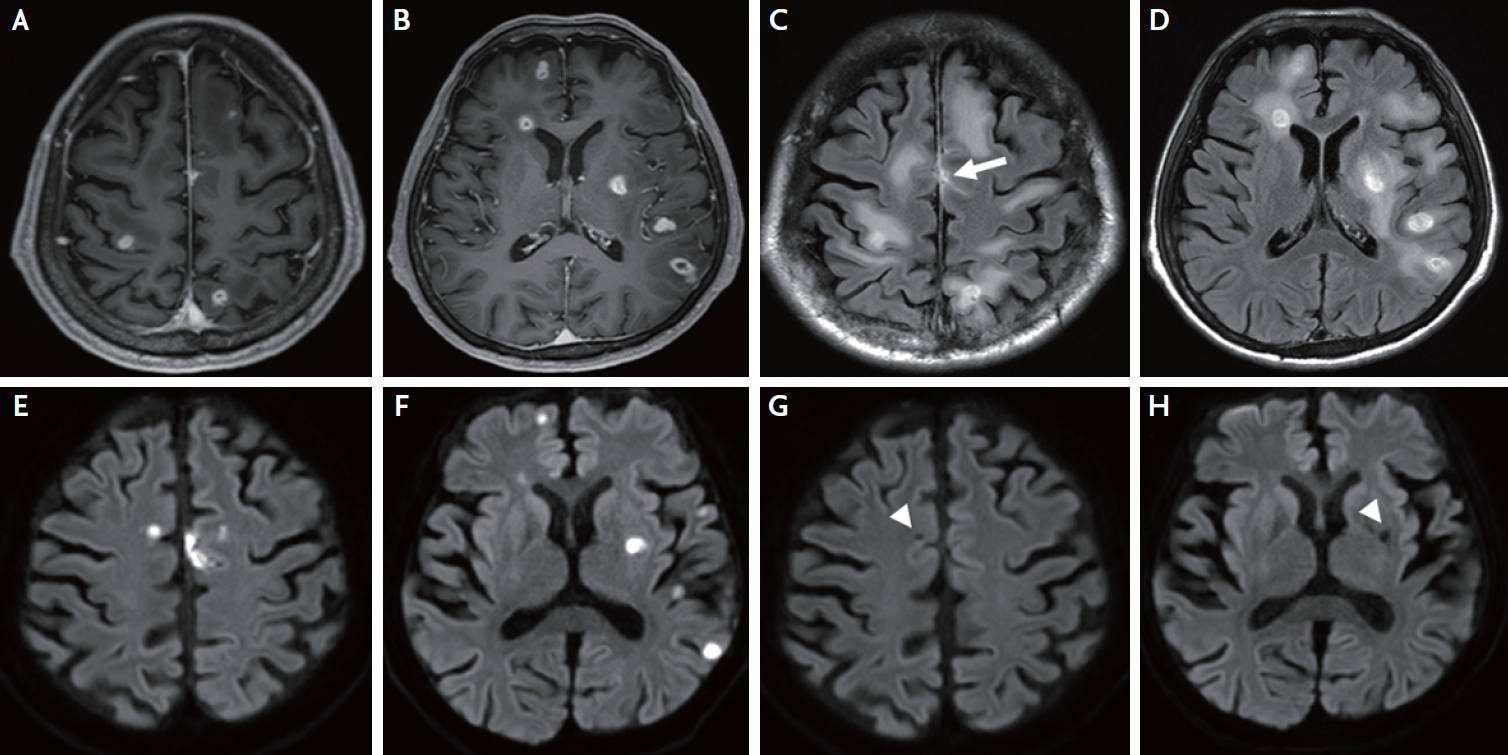
Multiple brain abscesses on magnetic resonance images. (A, B) Axial contrast-enhanced T1-weighted image shows multiple ring-enhancing lesions in the right frontal cortex and subcortex, left frontal, parietal, temporal, insular cortex, and basal ganglia. (C, D) Axial contrast-enhanced T2-fluid attenuated inversion recovery image shows multiple ring-enhancing lesions in the right frontal cortex and subcortex, left frontal, parietal, temporal, insular cortex, and basal ganglia and meningeal enhancement at the left medial frontal sulci (white arrow) with surrounding edema. (E, F) Hyperintense lesions in the right frontal cortex and subcortex, left frontal, temporal, insular, parietal cortex, and basal ganglia on diffusion weighted image. (G, H) Resolved hyperintense lesions (white arrowheads) in the right frontal cortex and subcortex, left frontal, temporal, insular, parietal cortex, and basal ganglia on diffusion-weighted images after antibiotic treatment.
DISCUSSION
We present a case of Klebsiella meningitis associated with brain abscess and endophthalmitis in a 58-year-old man with alcoholic liver cirrhosis and hepatocellular carcinoma who presented with fever, right eyeball pain, vision loss, and persistent headache.
The prevalence of brain abscess is 0.3–0.9 patients per 100,000 population worldwide. The incidence is higher in developing countries than in developed countries.5 In particular, brain abscesses are common in males and immunocompromised patients. The mortality rate of brain abscess is approximately 10–40% and the prognosis of brain abscess varies depending on the etiology, so if a brain abscess and meningitis are diagnosed, we should search for combined infection of other organs and perform appropriate and prompt treatment.6 Depending on the route of infection, brain abscesses can be divided into adjacent site infections, such as oropharynx abscesses or paranasal sinus abscesses, hematogenous spread from valvular heart disease or lung disease, or direct spread by operative procedures or trauma.6 Bacteria causing brain abscesses include Streptococcus species (34%), Staphylococcus species (18%), Proteus species (7%) and Klebsiella pneumoniae (2%).7 Brain abscesses caused by Klebsiella pneumoniae are frequently observed in patients with chronic alcoholism, liver cirrhosis, diabetes mellitus, and chronic otitis media.8 Compared with liver abscesses due to non-Klebsiella pneumoniae, liver abscesses due to Klebsiella pneumoniae rarely have biliary or portal vein routes of infection involving hepatobiliary disease and commonly have distant metastases to the eye or brain via the bloodstream, thus causing endophthalmitis or brain abscess. Klebsiella pneumoniae causes 50–88% of pyogenic liver abscesses; however, the patient in this case developed a brain abscess and meningitis without a liver abscess. Although the initial brain CT showed no abnormal findings and empirical antibiotic treatment for Klebsiella pneumoniae was performed, persistent headache occurred on the seventh day after admission, and a brain abscess and meningitis were diagnosed on subsequent brain MRI. Therefore, we believe that our patient developed a brain abscess and meningitis due to Klebsiella pneumoniae infection via the bloodstream. Although the location of the abscesses varied with etiology, lesions were typically located in the temporal lobe and cerebellum,9 as in our report.
Endophthalmitis caused by Klebsiella pneumoniae is rare, but often progresses quickly and has a very poor prognosis. Our patient was continuously treated with antibiotics at the time of admission, but vision loss due to endophthalmitis did not resolve until discharge. Endophthalmitis is usually associated with primary liver abscess and has also been reported to be associated with urinary tract infection, kidney abscess, and prostate abscess.10 Our patient had both alcoholic liver cirrhosis and a urinary tract infection. Endophthalmitis caused by Klebsiella pneumoniae should be considered if a patient with Klebsiella pneumoniae infection complains of blurred vision, reduced vision, or eye pain in one or both eyes, as in our patient.
Treatment of brain abscess and endophthalmitis caused by Klebsiella pneumoniae should include antibiotic treatment, surgical treatment if necessary, and removal of the primary lesion. It is known that old age, neurological deficits at admission, and diabetes mellitus are important prognostic factors.8 Because the size of multiple brain abscesses appeared very small on brain MRI, we decided to treat the patient with antibiotics only; multiple brain abscesses were resolved. Klebsiella pneumoniae infection often causes metastatic lesions; therefore, if a patient with Klebsiella pneumoniae infection has fever and headache, the possibility of a brain abscess and meningitis should be considered.
Notes
Ethics statement
This case report was approved by the Research Ethics Committee of the Kyung Hee University Hospital (Approval No. KHUH IRB 2020-08-011). The IRB of Kyung Hee University Hospital waived the need for informed consent.
Availability of Data and Material
All data related to this study are included in the main text.
Sources of Funding
This research was supported by a grant from Kyung Hee University in 2022 (grant number: KHU- 20220786) and a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HI20C1405).
Conflicts of Interest
No potential conflicts of interest relevant to this article was reported.
Acknowledgements
None.
