Atypical Manifestation of Zoster Meningitis Presented with Headache and Multiple Cerebral Vasoconstrictions
Article information
Abstract
Reversible cerebral vasoconstriction syndrome (RCVS) is characterized by headaches and multiple transient cerebral vasoconstrictions. Central nervous system (CNS) infections related to the varicella zoster virus (VZV) can complicate various neurological disorders, including cerebral vasculopathy. We present the case of a patient who complained of a severe headache without any other symptoms or focal neurological signs. Brain magnetic resonance angiography showed multiple focal stenoses, especially in the right middle cerebral artery (MCA), and transcranial Doppler sonography revealed increased velocities in the MCA and right anterior cerebral artery. Initially, the headache was attributed to RCVS, and nimodipine infusion was initiated; however, the headache worsened. A cerebrospinal fluid study showed pleocytosis, increased protein levels, and positive polymerase chain reaction markers for VZV. No skin lesions or fever were observed during treatment. Our case emphasizes considering VZV meningitis as a cause of cerebral vasoconstriction, even in the absence of typical signs of CNS infection.
Acute headaches that are unresponsive to analgesics require prompt investigation for the diagnosis of structural brain disorders. Potentially important considerations include stroke, central nervous system (CNS) infection, and reversible cerebral vasoconstriction syndrome (RCVS). RCVS is characterized by recurrent headache and transient multiple segmental vasoconstrictions of cerebral arteries known as “strings and beads” appearance.1,2 The repetitive cerebrovascular constriction and dilatation seen in RCVS tend to improve within 1–3 months, and the typical headache pattern is a thunderclap headache that lasts for a few hours.1,2 A critical assessment for the diagnosis of RCVS is a cerebrospinal fluid (CSF) study to exclude CNS infection/ inflammation. CNS infection related to varicella zoster virus (VZV) can complicate various neurological disorders, even in immunocompetent patients, including those with cerebral vasculopathies.3 We report the case of an atypical vascular manifestation of VZV meningitis clinically suspected as RCVS.
CASE
A 26-year-old male visited our outpatient clinic complaining of a headache that started abruptly and recurred 5 days after swimming. He had no history of underlying diseases, medications, or trauma. The headache was pulsatile, located in both frontal areas, with severe intensities corresponding to a visual analog scale (VAS) score of 10, and did not respond to any analgesics. No significant exacerbation of headaches was observed with coughing, defecation, or maneuvers such as the Valsalva maneuver or positional changes. On admission, physical and neurological examination results were normal, and laboratory blood findings were unremarkable, including normal erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) values. His initial vital signs were as follows: blood pressure, 130/80 mmHg; heart rate, 80 beats/min; and body temperature, 36.7°C. Brain magnetic resonance imaging (MRI) revealed no acute lesions, abnormal contrast-enhancement findings, or lesions suggestive of other neurological diseases. Brain MR angiography (MRA) showed multiple focal stenoses, especially in the right proximal middle cerebral artery (MCA). Transcranial Doppler sonography (TCD) revealed increased velocities in both the MCA (asymmetrically higher on the right side) and right anterior cerebral artery (Fig. 1). Under the clinically suspected diagnosis of RCVS, intravenous nimodipine treatment was initiated. Despite receiving medication, his headache worsened. On the third day of admission, he developed transient confusion. A lumbar puncture showed elevated opening pressure (>40 cmH2O), white blood cell (WBC) count (637 WBCs/mm3, lymphocyte-dominant [89.2%]), and protein levels (95.2 mg/dL) suggestive of CNS infection. Other CSF profiles were as follows: red blood cell (RBC) counts (1 RBC/mm3); glucose (49 mg/dL); adenosine deaminase (12); tuberculosis polymerase chain reaction (PCR; negative); infectious markers (PCR, culture) including fungus, bacteria, and virus except the VZV (all negative); VZV immunoglobulin M (negative); and VZV immunoglobulin G (positive). PCR markers for VZV were positive in the CSF, and treatments were modified according to the CSF findings; intravenous acyclovir (10 mg/kg 3 times/day for 10 days) and dexamethasone (5 mg 3 times/day for 5 days) were initiated. The confusion disappeared the next day, and the headache improved to a mild intensity on the third day of treatment. During the course of treatment, skin lesions suggestive of varicella zoster infection, fever, or meningismus were not identified. The symptoms improved and the patient was discharged without any neurological deficits.
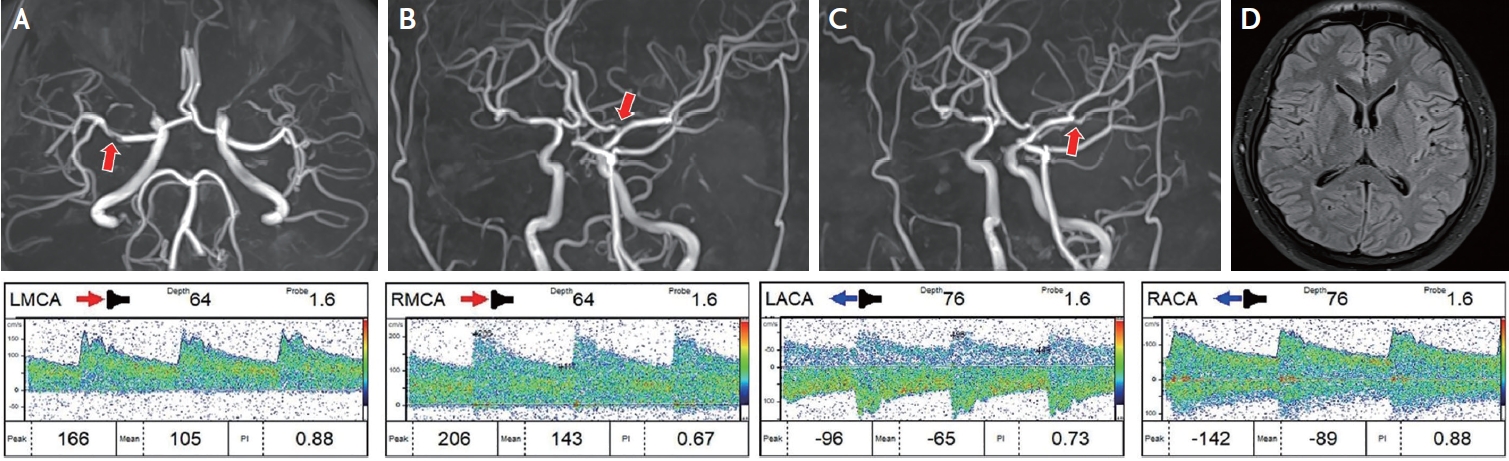
Neuroimaging and transcranial Doppler sonography findings. Upper: brain MRA showing right MCA focal stenosis (A). Additionally, mild focal stenosis of the left ACA, and (B) left MCA stenosis (C) is also observed. FLAIR showed no structural lesion (D). Lower: TCD showing increased velocities in both the MCA and ACA. ACA, anterior cerebral artery; MCA, middle cerebral artery; MRA, magnetic resonance angiography; TCD, transcranial Doppler sonography; FLAIR, fluid-attenuated inversion recovery.
DISCUSSION
Herein, we report the case of an atypical zoster meningitis vasculopathy. The patient complained of severe recurrent headaches that occurred after swimming. No findings suggested CNS infection. The patient was young and had no underlying diseases, and MRA/TCD findings suggested multiple focal stenoses; hence, RCVS was initially suggested. Subsequently, the patient was diagnosed with vasculopathy caused by herpes zoster meningitis.
VZV, an alpha herpesvirus, causes chicken pox during childhood and subsequently becomes latent in the neurons of the cranial and spinal ganglia in most patients without evident signs or symptoms.3 VZV has the potential to reactivate, resulting in a dermatomal rash with neuralgic pain, and its most common complication is meningitis.4 In patients who are immunocompetent, it can spread to intracranial vessels, usually involving the large arteries, while in patients who are immunocompromised, it presents more severe manifestations such as ventriculitis, encephalitis, or myelitis.3 Direct spread to the intracranial arteries via the trigeminovascular connections or hematogenous seeding via the sympathetic nervous system are possible mechanisms for the intracranial involvement of VZV.3 VZV vasculopathy may induce functional damage in the vascular endothelium, leading to thrombosis, stenosis, occlusion, or intracranial hemorrhage.3,4 Additionally, VZV vasculopathy can affect patients who are immunocompetent and those who are immunocompromised, manifests either unifocally or multifocally, develops without a rash, and often coexists with VZV meningitis, radiculitis, and myelitis.4 Thus, the diagnosis of VZV vasculopathy is challenging as it requires differentiation from other neurological disorders such as CNS vasculitis, atherosclerosis, and other CNS infections such as neurosyphilis and RCVS.4 Confirmation of VZV in the CSF is necessary to diagnose VZV vasculopathy.4
In a previous report by Singhal et al.5, most cases (78%) of RCVS showed normal CSF findings, with only 3% exhibiting pleocytosis greater than 10 WBCs/mm3.6 Consequently, most CSF analyses in patients with RCVS are nearly normal,5,7 and reversibility of vasoconstriction is not confirmed through follow up. We initially concluded that the present case did not sufficiently meet the diagnostic criteria of RCVS. As the patient’s symptoms improved and the outpatient visit was complete, follow-up TCD/MRA to assess the reversibility of vasoconstriction was not feasible. We considered the focal stenosis a transient vasculopathy related to VZV meningitis, given that the headache disappeared and the patient did not show any neurological symptoms.
Our case highlights the possibility of VZV meningitis as a cause of cerebral vasculopathies and headaches, even in the absence of typical signs of CNS infections. While VZV meningitis without skin lesions or fever has rarely been reported in patients who are immunocompetent7,8 it can manifest with various clinical presentations. Therefore, CSF studies should be considered in patients who have headaches but do not respond adequately to conservative management.
Notes
Ethics Statement
This study was approved by the Institutional Review Board of Uijeongbu St. Mary's Hospital, Catholic University of Korea with a waiver for informed consent.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author upon reasonable request.
Sources of Funding
None.
Conflicts of Interest
No potential conflicts of interest relevant to this article were reported.
Acknowledgements
None.
