Cerebral arteriovenous malformation (AVM) is a disease characterized by a complex tangled web of abnormal vascular connections between the arterial feeders and the draining veins.1 AVMs are associated with high morbidity and mortality, mainly due to hemorrhagic complications.
Vascular steal is a complicated phenomenon that is associated with cerebral AVM.2 However, vascular steal in cerebral AVM very rarely causes ischemic stroke, and only a few such cases have been reported.3 Here, we describe a unique case of cerebral AVM presenting as acute lacunar-like infarction, presumably resulting from vascular steal.
CASE
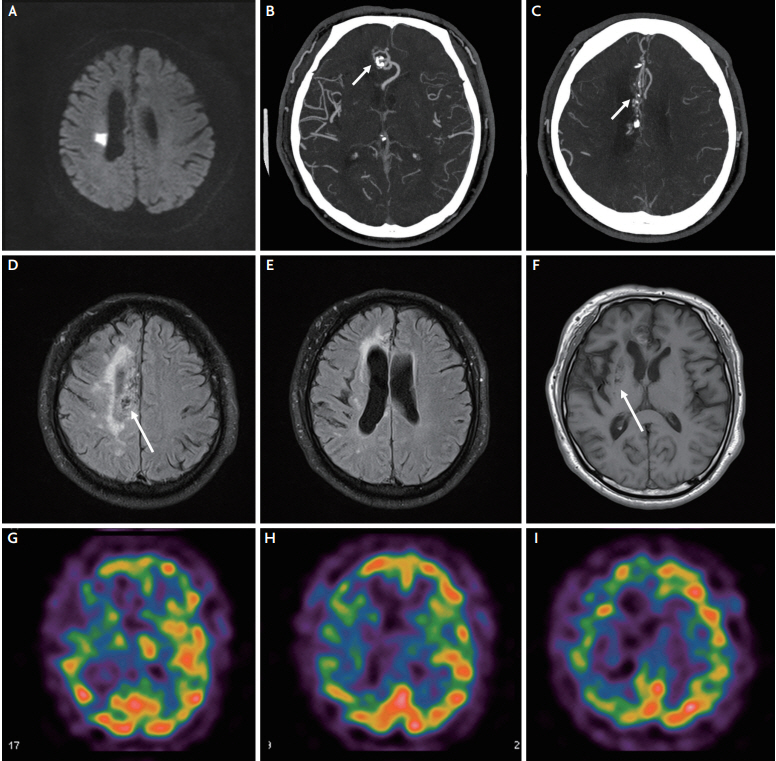
A 46-year-old hypertensive, but otherwise healthy, man presented with a 2-day history of dysarthria and left hemiparesis of sudden onset. On admission, he was not on antihypertensive medication, and his blood pressure was 157/128 mmHg. Initial neurological examination showed dysarthria, left central-type facial palsy, and left hemiparesis (Medical Research Council [MRC] motor grade IV). Diffusion-weighted magnetic resonance imaging (MRI) revealed an acute, small, solitary infarct in the right corona radiata (Fig. 1A). Therefore, he was initially diagnosed with acute lacunar infarction, and was treated with 100 mg aspirin and 40 mg atorvastatin. Subsequently, head-and-neck computed tomographic angiography revealed normal vessels, apart from an AVM with calcification in the right corpus callosum and cingulate gyrus (Fig. 1B, C). Additional MRI sequences were acquired, which showed multiple flow voids corresponding to the AVM (Fig. 1D, arrow), and revealed chronic white matter hyperintensities and multiple chronic lacunar infarcts with mild cortical atrophy and ventricular dilatation in the right cerebral hemisphere (Fig. 1E, F). However, there were no definite ischemic lesions in the left cerebral hemisphere. Technetium-99m-ethyl cysteinate dimer single-photon emission computed tomography showed diffuse hypoperfusion in the right cerebral hemisphere (Fig. 1G-I).
He underwent heart examinations, including transthoracic echocardiography and 24-hour Holter monitoring, all of which had normal results. His clinical course during admission was stable with aspirin and statin treatment. However, there was not much improvement in his hemiparesis.
He refused further investigations, such as catheter angiography, and was discharged from the hospital on the 7th day. At the 6-month follow-up, he still had left hemiparesis (MRC motor grade IV) with a modified Rankin scale score of 2.
DISCUSSION
Cerebral AVM usually manifests as hemorrhage or seizure.1 Focal neurological deficits due to cerebral infarction are quite rare (<0.1%).4 Previous studies have reported large artery territory infarcts associated with AVM.3-5 Unlike the previous studies, the present case uniquely manifested as an acute lacunar-like, that is, a small, solitary infarct.
Cerebral infarction associated with AVM may result from various etiologies, including coincidental cardioembolic or atherothrombotic lesions,4,5 steno-occlusion of a feeding artery due to fibromuscular proliferation or endothelial injury associated with turbulent high velocity blood flow,4,6,7 or vascular steal, which diverts blood flow from adjacent brain tissue into the low resistance network of the AVM.3 Although hypertension might have predisposed our patient to the “lacunar” infarct in this case, hypoperfusion associated with vascular steal could have contributed much more to the development of the lesion, given the imaging findings of chronic ischemia exclusively involving the right hemisphere around the AVM with sparing of the left hemisphere.