1. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al.; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2020 update: A report from the American Heart Association.
Circulation. 2020;141:e139-e596.

2. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019.
Lancet Neurol. 2021;20:795-820.


5. Tsivgoulis G, Kargiotis O, Alexandrov AV. Intravenous thrombolysis for acute ischemic stroke: a bridge between two centuries.
Expert Rev Neurother. 2017;17:819-837.


6. Psychogios K, Tsivgoulis G. Intravenous thrombolysis for acute ischemic stroke: why not?
Curr Opin Neurol. 2022;35:10-17.


8. Joo H, Wang G, George MG. Use of intravenous tissue plasminogen activator and hospital costs for patients with acute ischaemic stroke aged 18-64 years in the USA.
Stroke Vasc Neurol. 2016;1:8-15.



9. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al.; American Heart Association Stroke Council. 2018 Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association.
Stroke. 2018;49:e46-e110.


10. Bivard A, Parsons M. Tissue is more important than time: insights into acute ischemic stroke from modern brain imaging.
Curr Opin Neurol. 2018;31:23-27.


11. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al.; HERMES Collaborators. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: A meta-analysis.
JAMA. 2016;316:1279-1288.


12. Desai SM, Rocha M, Jovin TG, Jadhav AP. High variability in neuronal loss.
Stroke. 2019;50:34-37.


13. Rocha M, Jovin TG. Fast versus slow progressors of infarct growth in large vessel occlusion stroke: Clinical and research implications.
Stroke. 2017;48:2621-2627.


14. Chalela JA, Kidwell CS, Nentwich LM, Luby M, Butman JA, Demchuk AM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison.
Lancet. 2007;369:293-298.



15. Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score.
Lancet. 2000;355:1670-1674.

16. Coutts SB, Demchuk AM, Barber PA, Hu WY, Simon JE, Buchan AM, et al.; VISION Study Group. Interobserver variation of ASPECTS in real time.
Stroke. 2004;35:e103-e105.


18. Mayer SA, Viarasilpa T, Panyavachiraporn N, Brady M, Scozzari D, Van Harn M, et al. CTA-for-All: Impact of emergency computed tomographic angiography for all patients with stroke presenting within 24 hours of onset.
Stroke. 2020;51:331-334.


19. Goyal MS, Hoff BG, Williams J, Khoury N, Wiesehan R, Heitsch L, et al. Streamlined hyperacute magnetic resonance imaging protocol identifies tissue-type plasminogen activator-eligible stroke patients when clinical impression is stroke mimic.
Stroke. 2016;47:1012-1017.



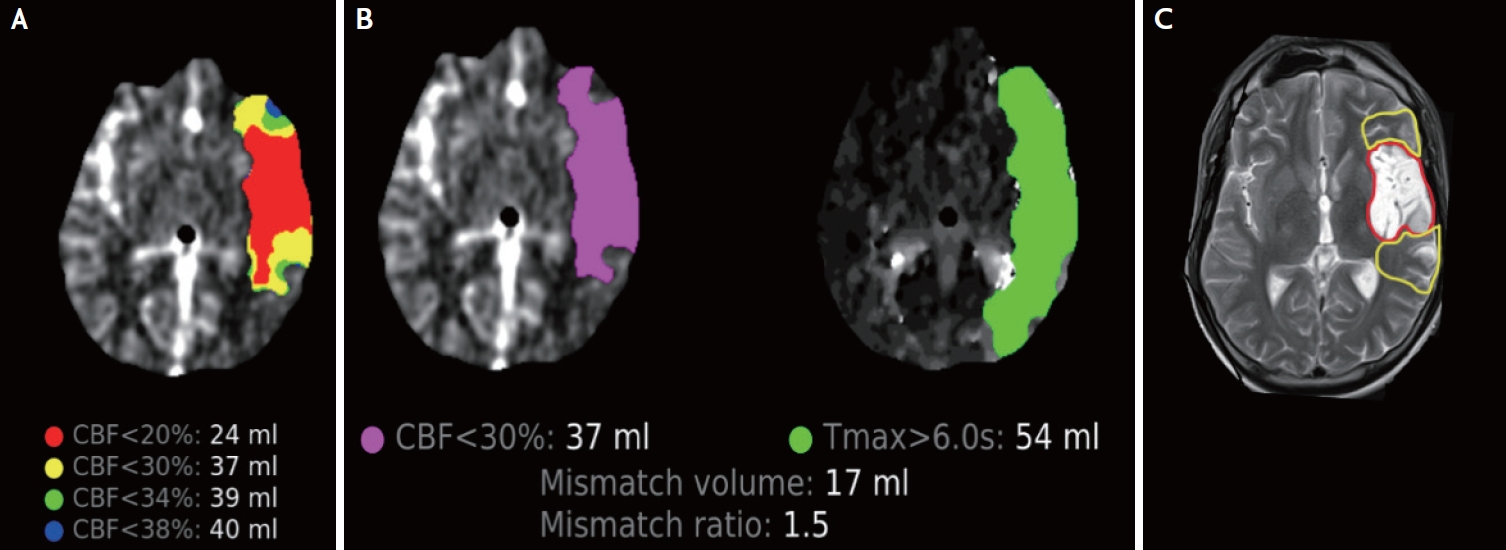
20. Demeestere J, Wouters A, Christensen S, Lemmens R, Lansberg MG. Review of perfusion imaging in acute ischemic stroke: From time to tissue.
Stroke. 2020;51:1017-1024.


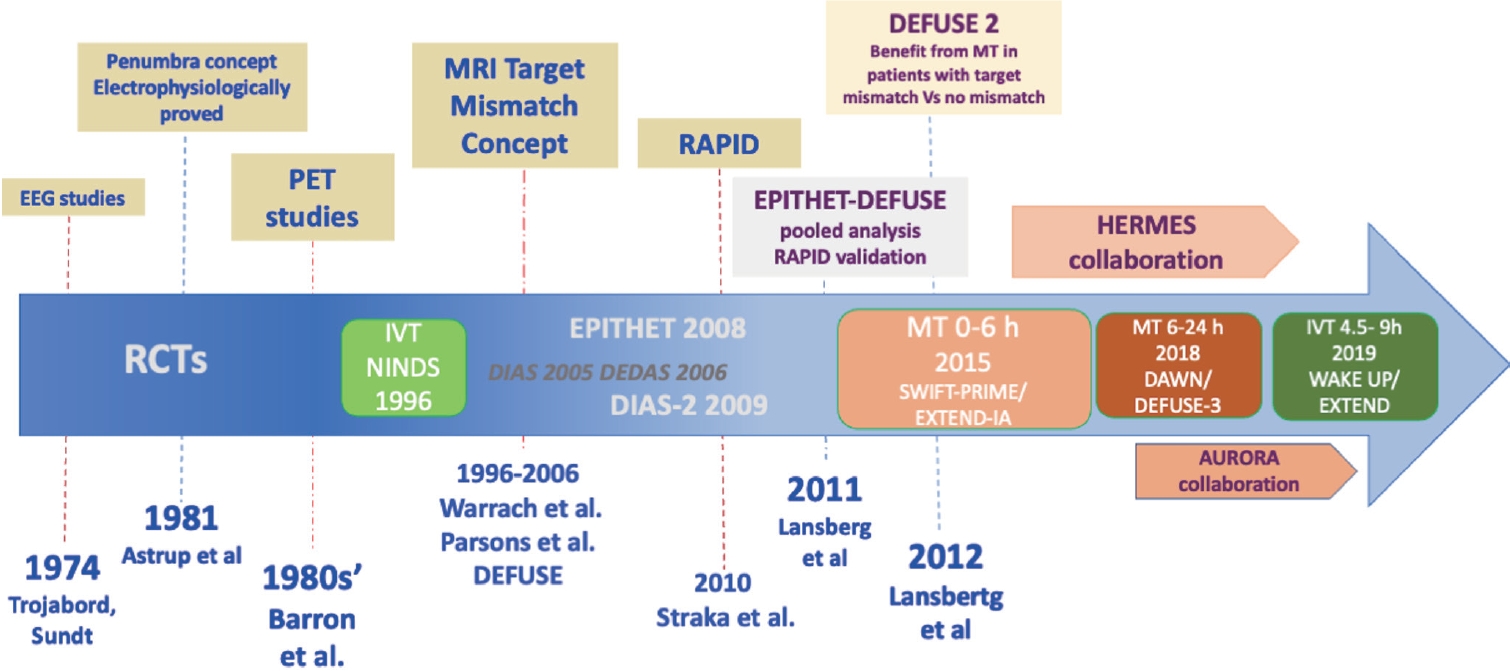
21. Astrup J, Siesjö BK, Symon L. Thresholds in cerebral ischemia - the ischemic penumbra.
Stroke. 1981;12:723-725.


22. Trojaborg W, Boysen G. Relation between EEG, regional cerebral blood flow and internal carotid artery pressure during carotid endarterectomy.
Electroencephalogr Clin Neurophysiol. 1973;34:61-69.


23. Sundt TM Jr, Sharbrough FW, Anderson RE, Michenfelder JD. Cerebral blood flow measurements and electroencephalograms during carotid endarterectomy.
J Neurosurg. 1974;41:310-320.


24. Astrup J, Symon L, Branston NM, Lassen NA. Cortical evoked potential and extracellular K+ and H+ at critical levels of brain ischemia.
Stroke. 1977;8:51-57.


25. Branston NM, Strong AJ, Symon L. Extracellular potassium activity, evoked potential and tissue blood flow. Relationships during progressive ischaemia in baboon cerebral cortex.
J Neurol Sci. 1977;32:305-321.

26. Jones TH, Morawetz RB, Crowell RM, Marcoux FW, FitzGibbon SJ, DeGirolami U, et al. Thresholds of focal cerebral ischemia in awake monkeys.
J Neurosurg. 1981;54:773-782.


27. Baron JC, Bousser MG, Comar D, Soussaline F, Castaigne P. Noninvasive tomographic study of cerebral blood flow and oxygen metabolism in vivo. Potentials, limitations, and clinical applications in cerebral ischemic disorders.
Eur Neurol. 1981;20:273-284.



28. Baron JC. Mapping the ischaemic penumbra with PET: implications for acute stroke treatment.
Cerebrovasc Dis. 1999;9:193-201.



29. Ermine CM, Bivard A, Parsons MW, Baron JC. The ischemic penumbra: From concept to reality.
Int J Stroke. 2021;16:497-509.



30. Marchal G, Beaudouin V, Rioux P, de la Sayette V, Le Doze F, Viader F, et al. Prolonged persistence of substantial volumes of potentially viable brain tissue after stroke: a correlative PET-CT study with voxel-based data analysis.
Stroke. 1996;27:599-606.


31. Heiss WD, Huber M, Fink GR, Herholz K, Pietrzyk U, Wagner R, et al. Progressive derangement of periinfarct viable tissue in ischemic stroke.
J Cereb Blood Flow Metab. 1992;12:193-203.



32. Warach S. Measurement of the ischemic penumbra with MRI: it’s about time.
Stroke. 2003;34:2533-2534.


33. Warach S, Dashe JF, Edelman RR. Clinical outcome in ischemic stroke predicted by early diffusion-weighted and perfusion magnetic resonance imaging: a preliminary analysis.
J Cereb Blood Flow Metab. 1996;16:53-59.



34. Hjort N, Christensen S, Sølling C, Ashkanian M, Wu O, Røhl L, et al. Ischemic injury detected by diffusion imaging 11 minutes after stroke.
Ann Neurol. 2005;58:462-465.


35. Kidwell CS, Saver JL, Mattiello J, Starkman S, Vinuela F, Duckwiler G, et al. Thrombolytic reversal of acute human cerebral ischemic injury shown by diffusion/perfusion magnetic resonance imaging.
Ann Neurol. 2000;47:462-469.


36. Lakomkin N, Pan J, Stein L, Malkani B, Dhamoon M, Mocco J. Diffusion MRI reversibility in ischemic stroke following thrombolysis: A meta-analysis.
J Neuroimaging. 2020;30:471-476.



38. Campbell BCV, Lansberg MG, Broderick JP, Derdeyn CP, Khatri P, Sarraj A, et al.; STAIR XI Consortium. Acute stroke imaging research roadmap IV: Imaging selection and outcomes in acute stroke clinical trials and practice.
Stroke. 2021;52:2723-2733.



39. Chalela JA, Kang DW, Luby M, Ezzeddine M, Latour LL, Todd JW, et al. Early magnetic resonance imaging findings in patients receiving tissue plasminogen activator predict outcome: Insights into the pathophysiology of acute stroke in the thrombolysis era.
Ann Neurol. 2004;55:105-112.


40. Parsons MW, Barber PA, Chalk J, Darby DG, Rose S, Desmond PM, et al. Diffusion- and perfusion-weighted MRI response to thrombolysis in stroke.
Ann Neurol. 2002;51:28-37.


41. Albers GW, Thijs VN, Wechsler L, Kemp S, Schlaug G, Skalabrin E, et al. Magnetic resonance imaging profiles predict clinical response to early reperfusion: the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study.
Ann Neurol. 2006;60:508-517.



42. Davis SM, Donnan GA, Parsons MW, Levi C, Butcher KS, Peeters A, et al.; EPITHET investigators. Effects of alteplase beyond 3 h after stroke in the Echoplanar Imaging Thrombolytic Evaluation Trial (EPITHET): a placebo-controlled randomised trial.
Lancet Neurol. 2008;7:299-309.


43. Hacke W, Furlan AJ, Al-Rawi Y, Davalos A, Fiebach JB, Gruber F, et al. Intravenous desmoteplase in patients with acute ischaemic stroke selected by MRI perfusion-diffusion weighted imaging or perfusion CT (DIAS-2): a prospective, randomised, double-blind, placebo-controlled study.
Lancet Neurol. 2009;8:141-150.


44. Hacke W, Albers G, Al-Rawi Y, Bogousslavsky J, Davalos A, Eliasziw M, et al.; DIAS Study Group. The Desmoteplase in Acute Ischemic Stroke Trial (DIAS): a phase II MRI-based 9-hour window acute stroke thrombolysis trial with intravenous desmoteplase.
Stroke. 2005;36:66-73.


45. Furlan AJ, Eyding D, Albers GW, Al-Rawi Y, Lees KR, Rowley HA, et al.; DEDAS Investigators. Dose Escalation of Desmoteplase for Acute Ischemic Stroke (DEDAS): evidence of safety and efficacy 3 to 9 hours after stroke onset.
Stroke. 2006;37:1227-1231.


46. Donnan GA, Davis SM. Life after DIAS II.
Int J Stroke. 2007;2:236-237.



47. Mishra NK, Albers GW, Davis SM, Donnan GA, Furlan AJ, Hacke W, et al. Mismatch-based delayed thrombolysis: a meta-analysis.
Stroke. 2010;41:e25-33.

48. Albers GW, Fisher M. Improving the accuracy of perfusion imaging in acute ischemic stroke.
Ann Neurol. 2011;70:347-349.


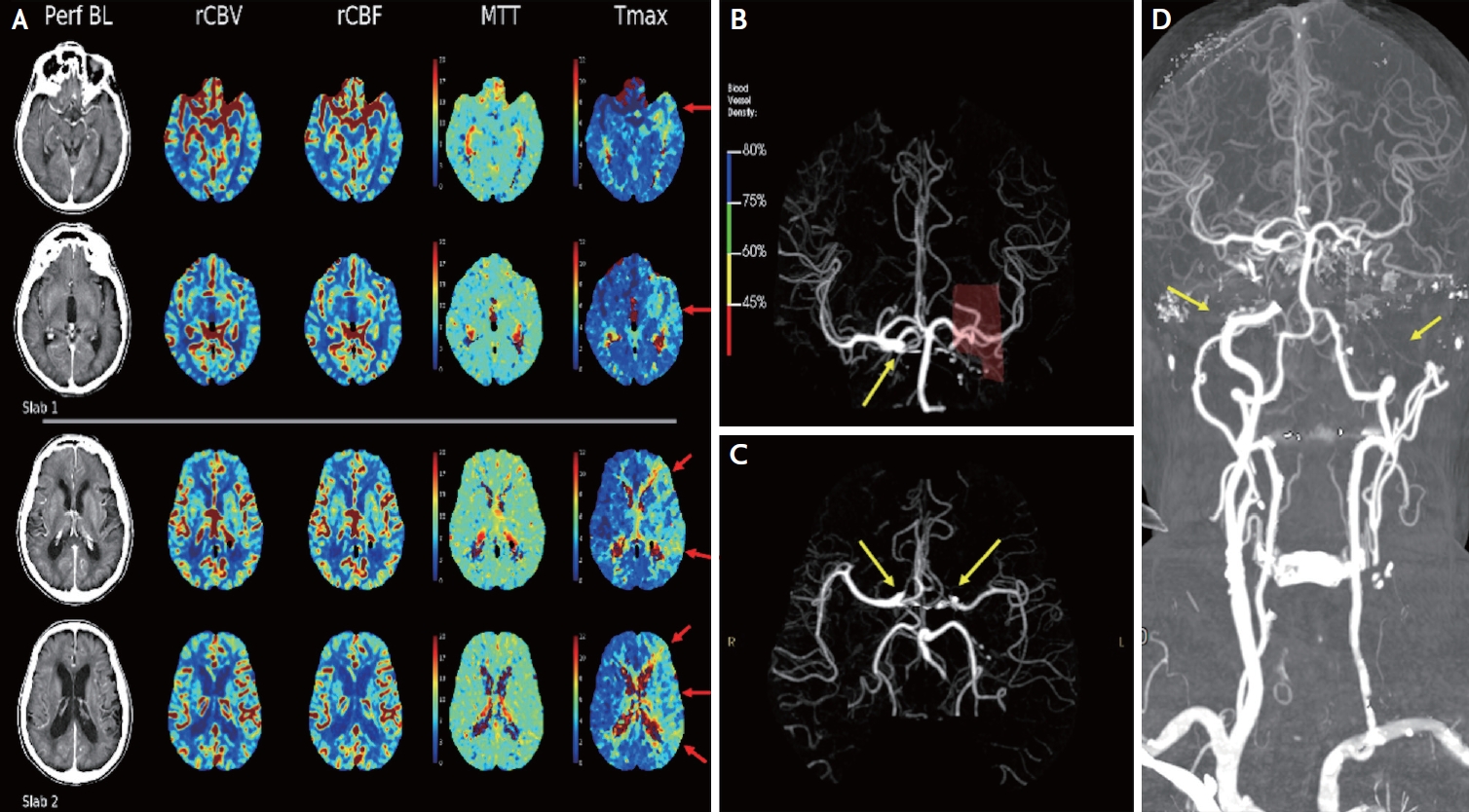
49. Tong E, Sugrue L, Wintermark M. Understanding the neurophysiology and quantification of brain perfusion.
Top Magn Reson Imaging. 2017;26:57-65.


50. Essig M, Shiroishi MS, Nguyen TB, Saake M, Provenzale JM, Enterline D, et al. Perfusion MRI: the five most frequently asked technical questions.
AJR Am J Roentgenol. 2013;200:24-34.



51. McKinley R, Hung F, Wiest R, Liebeskind DS, Scalzo F. A Machine learning approach to perfusion imaging with dynamic susceptibility contrast MR.
Front Neurol. 2018;9:717.



52. Dani KA, Thomas RG, Chappell FM, Shuler K, MacLeod MJ, Muir K, et al.; Translational Medicine Research Collaboration Multicentre Acute Stroke Imaging Study. Computed tomography and magnetic resonance perfusion imaging in ischemic stroke: definitions and thresholds.
Ann Neurol. 2011;70:384-401.


53. Straka M, Albers GW, Bammer R. Real-time diffusion-perfusion mismatch analysis in acute stroke.
J Magn Reson Imaging. 2010;32:1024-1037.



54. Zaro-Weber O, Moeller-Hartmann W, Heiss WD, Sobesky J. Maps of time to maximum and time to peak for mismatch definition in clinical stroke studies validated with positron emission tomography.
Stroke. 2010;41:2817-2821.


55. Olivot JM, Mlynash M, Thijs VN, Kemp S, Lansberg MG, Wechsler L, et al. Optimal Tmax threshold for predicting penumbral tissue in acute stroke.
Stroke. 2009;40:469-475.



56. Lansberg MG, Lee J, Christensen S, Straka M, De Silva DA, Mlynash M, et al. RAPID automated patient selection for reperfusion therapy: a pooled analysis of the Echoplanar Imaging Thrombolytic Evaluation Trial (EPITHET) and the Diffusion and Perfusion Imaging Evaluation for Understanding Stroke Evolution (DEFUSE) Study.
Stroke. 2011;42:1608-1614.



57. Campbell BC, Christensen S, Levi CR, Desmond PM, Donnan GA, Davis SM, et al. Cerebral blood flow is the optimal CT perfusion parameter for assessing infarct core.
Stroke. 2011;42:3435-3440.


58. Kamalian S, Kamalian S, Maas MB, Goldmacher GV, Payabvash S, Akbar A, et al. CT cerebral blood flow maps optimally correlate with admission diffusion-weighted imaging in acute stroke but thresholds vary by postprocessing platform.
Stroke. 2011;42:1923-1928.



59. Campbell BC, Christensen S, Levi CR, Desmond PM, Donnan GA, Davis SM, et al. Comparison of computed tomography perfusion and magnetic resonance imaging perfusion-diffusion mismatch in ischemic stroke.
Stroke. 2012;43:2648-2653.


60. Bivard A, Levi C, Spratt N, Parsons M. Perfusion CT in acute stroke: a comprehensive analysis of infarct and penumbra.
Radiology. 2013;267:543-550.


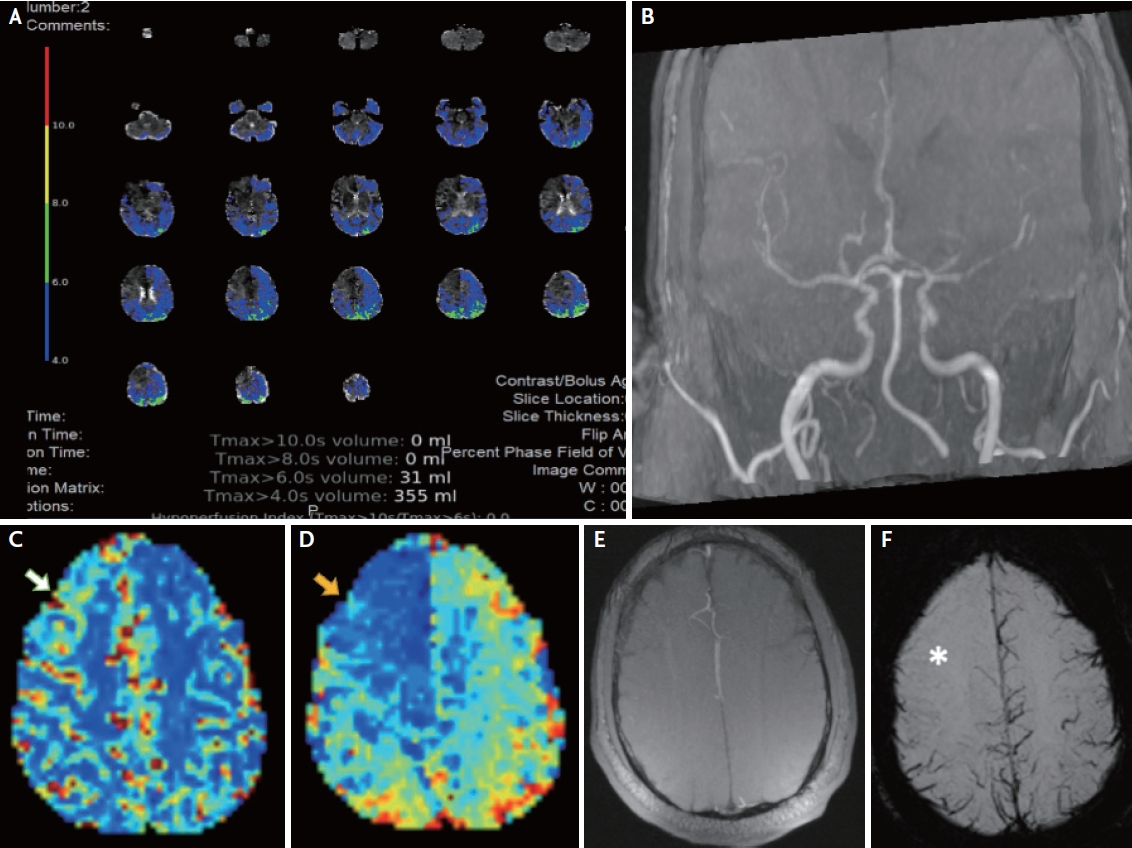
63. Lin L, Bivard A, Krishnamurthy V, Levi CR, Parsons MW. Whole-Brain CT perfusion to quantify acute ischemic penumbra and core.
Radiology. 2016;279:876-887.


64. Mokin M, Levy EI, Saver JL, Siddiqui AH, Goyal M, Bonafé A, et al.; SWIFT PRIME Investigators. Predictive value of RAPID assessed perfusion thresholds on final infarct volume in SWIFT PRIME (Solitaire With the Intention for Thrombectomy as Primary Endovascular Treatment).
Stroke. 2017;48:932-938.


65. Amukotuwa S, Straka M, Aksoy D, Fischbein N, Desmond P, Albers G, et al. Cerebral blood flow predicts the infarct core: New insights from contemporaneous diffusion and perfusion imaging.
Stroke. 2019;50:2783-2789.



66. Kudo K, Sasaki M, Østergaard L, Christensen S, Uwano I, Suzuki M, et al. Susceptibility of Tmax to tracer delay on perfusion analysis: quantitative evaluation of various deconvolution algorithms using digital phantoms.
J Cereb Blood Flow Metab. 2011;31:908-912.



69. García-Tornel Á, Campos D, Rubiera M, Boned S, Olivé-Gadea M, Requena M, et al. Ischemic core overestimation on computed tomography perfusion.
Stroke. 2021;52:1751-1760.


70. Sarraj A, Campbell BCV, Christensen S, Sitton CW, Khanpara S, Riascos RF, et al.; SELECT Investigators. Accuracy of CT perfusion-based core estimation of follow-up infarction: Effects of time since last known well.
Neurology. 2022;98:e2084-e2096.



71. Vagal A, Wintermark M, Nael K, Bivard A, Parsons M, Grossman AW, et al. Automated CT perfusion imaging for acute ischemic stroke: Pearls and pitfalls for real-world use.
Neurology. 2019;93:888-898.


72. Kargiotis O, Psychogios K, Safouris A, Andrikopoulou A, Eleftheriou A, Spiliopoulos S, et al. Computed tomography perfusion imaging in acute ischemic stroke: Accurate interpretation matters.
Stroke. 2023;54:e104-e108.


73. Ma H, Campbell BCV, Parsons MW, Churilov L, Levi CR, Hsu C, et al.; EXTEND Investigators. Thrombolysis guided by perfusion imaging up to 9 hours after onset of stroke.
N Engl J Med. 2019;380:1795-1803.

74. Ringleb P, Bendszus M, Bluhmki E, Donnan G, Eschenfelder C, Fatar M, et al.; ECASS-4 study group. Extending the time window for intravenous thrombolysis in acute ischemic stroke using magnetic resonance imaging-based patient selection.
Int J Stroke. 2019;14:483-490.



75. Thomalla G, Simonsen CZ, Boutitie F, Andersen G, Berthezene Y, Cheng B, et al.; WAKE-UP Investigators. MRI-guided thrombolysis for stroke with unknown time of onset.
N Engl J Med. 2018;379:611-622.


76. Campbell BCV, Ma H, Ringleb PA, Parsons MW, Churilov L, Bendszus M, et al.; EXTEND; ECASS-4; EPITHET Investigators. Extending thrombolysis to 4·5-9 h and wake-up stroke using perfusion imaging: a systematic review and meta-analysis of individual patient data.
Lancet. 2019;394:139-147.

77. Thomalla G, Boutitie F, Ma H, Koga M, Ringleb P, Schwamm LH, et al.; Evaluation of unknown Onset Stroke thrombolysis trials (EOS) investigators. Intravenous alteplase for stroke with unknown time of onset guided by advanced imaging: systematic review and meta-analysis of individual patient data.
Lancet. 2020;396:1574-1584.


78. Tsivgoulis G, Katsanos AH, Malhotra K, Sarraj A, Barreto AD, Köhrmann M, et al. Thrombolysis for acute ischemic stroke in the unwitnessed or extended therapeutic time window.
Neurology. 2020;94:e1241-e1248.


79. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 Update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association.
Stroke. 2019;50:e344-e418.


81. Macha K, Hoelter P, Siedler G, Knott M, Schwab S, Doerfler A, et al. Multimodal CT or MRI for IV thrombolysis in ischemic stroke with unknown time of onset.
Neurology. 2020;95:e2954-e2964.


83. Roaldsen MB, Eltoft A, Wilsgaard T, Christensen H, Engelter ST, Indredavik B, et al.; TWIST Investigators. Safety and efficacy of tenecteplase in patients with wake-up stroke assessed by non-contrast CT (TWIST): a multicentre, open-label, randomised controlled trial.
Lancet Neurol. 2023;22:117-126.

84. Tsivgoulis G, Katsanos AH, Sandset EC, Turc G, Nguyen TN, Bivard A, et al. Thrombolysis for acute ischaemic stroke: current status and future perspectives.
Lancet Neurol. 2023;22:418-429.


85. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al.; SWIFT PRIME Investigators. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke.
N Engl J Med. 2015;372:2285-2295.


86. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al.; EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection.
N Engl J Med. 2015;372:1009-1018.


87. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al.; ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke.
N Engl J Med. 2015;372:1019-1030.


88. Menon BK, d’Esterre CD, Qazi EM, Almekhlafi M, Hahn L, Demchuk AM, et al. Multiphase CT angiography: A new tool for the imaging triage of patients with acute ischemic stroke.
Radiology. 2015;275:510-520.


89. Evans JW, Graham BR, Pordeli P, Al-Ajlan FS, Willinsky R, Montanera WJ, et al.; ESCAPE Trial Investigators. Time for a time window extension: Insights from late presenters in the ESCAPE trial.
AJNR Am J Neuroradiol. 2018;39:102-106.



90. Wannamaker R, Guinand T, Menon BK, Demchuk A, Goyal M, Frei D, et al. Computed tomographic perfusion predicts poor outcomes in a randomized trial of endovascular therapy.
Stroke. 2018;49:1426-1433.


91. Kaschka IN, Kloska SP, Struffert T, Engelhorn T, Gölitz P, Kurka N, et al. Clot burden and collaterals in anterior circulation stroke: Differences between single-phase CTA and multi-phase 4D-CTA.
Clin Neuroradiol. 2016;26:309-315.



92. Tan Z, Parsons M, Bivard A, Sharma G, Mitchell P, Dowling R, et al. Comparison of computed tomography perfusion and multiphase computed tomography angiogram in predicting clinical outcomes in endovascular thrombectomy.
Stroke. 2022;53:2926-2934.


93. Tsivgoulis G, Katsanos AH, Schellinger PD, Köhrmann M, Caso V, Palaiodimou L, et al. Advanced neuroimaging in stroke patient selection for mechanical thrombectomy.
Stroke. 2018;49:3067-3070.


94. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al.; DAWN Trial Investigators. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct.
N Engl J Med. 2018;378:11-21.

95. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al.; DEFUSE 3 Investigators. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging.
N Engl J Med. 2018;378:708-718.



96. Jovin TG, Nogueira RG, Lansberg MG, Demchuk AM, Martins SO, Mocco J, et al. Thrombectomy for anterior circulation stroke beyond 6 h from time last known well (AURORA): a systematic review and individual patient data meta-analysis.
Lancet. 2022;399:249-258.


97. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al.; HERMES collaborators. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials.
Lancet. 2016;387:1723-1731.


98. Fransen PS, Berkhemer OA, Lingsma HF, Beumer D, van den Berg LA, Yoo AJ, et al.; Multicenter Randomized Clinical Trial of Endovascular Treatment of Acute Ischemic Stroke in the Netherlands Investigators. Time to reperfusion and treatment effect for acute ischemic stroke: A randomized clinical trial.
JAMA Neurol. 2016;73:190-196.

100. Berkhemer OA, Jansen IG, Beumer D, Fransen PS, van den Berg LA, Yoo AJ, et al.; MR CLEAN Investigators. Collateral status on baseline computed tomographic angiography and intra-arterial treatment effect in patients with proximal anterior circulation stroke.
Stroke. 2016;47:768-776.


101. Olthuis SGH, Pirson FAV, Pinckaers FME, Hinsenveld WH, Nieboer D, Ceulemans A, et al.; MR CLEAN-LATE investigators. Endovascular treatment versus no endovascular treatment after 6-24 h in patients with ischaemic stroke and collateral flow on CT angiography (MR CLEANLATE) in the Netherlands: a multicentre, open-label, blinded-endpoint, randomised, controlled, phase 3 trial.
Lancet. 2023;401:1371-1380.


102. Dittrich TD, Sporns PB, Kriemler LF, Rudin S, Nguyen A, Zietz A, et al. Mechanical thrombectomy versus best medical treatment in the late time window in Non-DEFUSENon-DAWN patients: A multicenter cohort study.
Stroke. 2023;54:722-730.



103. Nguyen TN, Abdalkader M, Nagel S, Qureshi MM, Ribo M, Caparros F, et al. Noncontrast computed tomography vs computed tomography perfusion or magnetic resonance imaging selection in late presentation of stroke with large-vessel occlusion.
JAMA Neurol. 2022;79:22-31.



104. Yoshimura S, Sakai N, Yamagami H, Uchida K, Beppu M, Toyoda K, et al. Endovascular therapy for acute stroke with a large ischemic region.
N Engl J Med. 2022;386:1303-1313.


105. Huo X, Ma G, Tong X, Zhang X, Pan Y, Nguyen TN, et al.; ANGEL-ASPECT Investigators. Trial of endovascular therapy for acute ischemic stroke with large infarct.
N Engl J Med. 2023;388:1272-1283.

106. Sarraj A, Hassan AE, Abraham MG, Ortega-Gutierrez S, Kasner SE, Hussain MS, et al.; SELECT2 Investigators. Trial of endovascular thrombectomy for large ischemic strokes.
N Engl J Med. 2023;388:1259-1271.

107. Fayad P. Improved prospects for thrombectomy in large ischemic stroke.
N Engl J Med. 2023;388:1326-1328.


109. Psychogios K, Safouris A, Kargiotis O, Magoufis G, Andrikopoulou A, Papageorgiou E, et al. Advanced neuroimaging preceding intravenous thrombolysis in acute ischemic stroke patients is safe and effective.
J Clin Med. 2021;10:2819.



110. Albers GW. Use of imaging to select patients for late window endovascular therapy.
Stroke. 2018;49:2256-2260.


111. Psychogios K, Kargiotis O, Safouris A, Magoufis G, Gelagoti M, Bonakis A, et al. Perfusion imaging averting intravenous thrombolysis in stroke mimics.
Neurol Sci. 2021;42:2591-2594.



112. Campbell BC, Weir L, Desmond PM, Tu HT, Hand PJ, Yan B, et al. CT perfusion improves diagnostic accuracy and confidence in acute ischaemic stroke.
J Neurol Neurosurg Psychiatry. 2013;84:613-618.


113. Siegler JE, Rosenberg J, Cristancho D, Olsen A, Pulst-Korenberg J, Raab L, et al. Computed tomography perfusion in stroke mimics.
Int J Stroke. 2020;15:299-307.



114. Campbell BCV, Majoie CBLM, Albers GW, Menon BK, Yassi N, Sharma G, et al.; HERMES collaborators. Penumbral imaging and functional outcome in patients with anterior circulation ischaemic stroke treated with endovascular thrombectomy versus medical therapy: a meta-analysis of individual patient-level data.
Lancet Neurol. 2019;18:46-55.

115. Olivot JM, Mlynash M, Inoue M, Marks MP, Wheeler HM, Kemp S, et al.; DEFUSE 2 Investigators. Hypoperfusion intensity ratio predicts infarct progression and functional outcome in the DEFUSE 2 Cohort.
Stroke. 2014;45:1018-1023.



116. Guenego A, Fahed R, Albers GW, Kuraitis G, Sussman ES, Martin BW, et al. Hypoperfusion intensity ratio correlates with angiographic collaterals in acute ischaemic stroke with M1 occlusion.
Eur J Neurol. 2020;27:864-870.



117. Guenego A, Marcellus DG, Martin BW, Christensen S, Albers GW, Lansberg MG, et al. Hypoperfusion intensity ratio is correlated with patient eligibility for thrombectomy.
Stroke. 2019;50:917-922.


118. van Horn N, Broocks G, Kabiri R, Kraemer MC, Christensen S, Mlynash M, et al. Cerebral hypoperfusion intensity ratio is linked to progressive early edema formation.
J Clin Med. 2022;11:2373.



119. Mohammaden MH, Haussen DC, Pisani L, Al-Bayati AR, Perry da Camara C, Bhatt N, et al. Baseline ASPECTS and hypoperfusion intensity ratio influence the impact of first pass reperfusion on functional outcomes.
J Neurointerv Surg. 2021;13:124-129.


120. Wu RR, Lu SS, Cao YZ, Xu XQ, Jia ZY, Zhao LB, et al. Hypoperfusion intensity ratio correlates with clinical outcome of endovascular thrombectomy in acute ischaemic stroke patients with late therapeutic window.
Clin Radiol. 2022;77:570-576.


121. Seners P, Scheldeman L, Christensen S, Mlynash M, Ter Schiphorst A, Arquizan C, et al.; Infarct-Growth Collaborators. Determinants of infarct core growth during inter-hospital transfer for thrombectomy.
Ann Neurol. 2023;93:1117-1129.



122. Guenego A, Mlynash M, Christensen S, Kemp S, Heit JJ, Lansberg MG, et al. Hypoperfusion ratio predicts infarct growth during transfer for thrombectomy.
Ann Neurol. 2018;84:616-620.



123. Jeong HG, Kim BJ, Kim H, Jung C, Han MK, Liebeskind DS, et al. Blood pressure drop and penumbral tissue loss in nonrecanalized emergent large vessel occlusion.
Stroke. 2019;50:2677-2684.


125. Parthasarathy R, Sohn SI, Jeerakathil T, Kate MP, Mishra SM, Nambiar VK, et al. A combined arterial and venous grading scale to predict outcome in anterior circulation ischemic stroke.
J Neuroimaging. 2015;25:969-977.



126. van Horn N, Heit JJ, Kabiri R, Broocks G, Christensen S, Mlynash M, et al. Venous outflow profiles are associated with early edema progression in ischemic stroke.
Int J Stroke. 2022;17:1078-1084.



127. MacLellan A, Mlynash M, Kemp S, Ortega-Gutierrez S, Heit JJ, Marks MP, et al.; DEFUSE 3 Investigators. Perfusion imaging collateral scores predict infarct growth in non-reperfused DEFUSE 3 patients.
J Stroke Cerebrovasc Dis. 2022;31:106208.


128. Sarraj A, Hassan AE, Grotta J, Blackburn S, Day A, Abraham M, et al.; SELECT Investigators. Early infarct growth rate correlation with endovascular thrombectomy clinical outcomes: Analysis from the SELECT study.
Stroke. 2021;52:57-69.


129. Lin L, Zhang H, Liu F, Chen C, Chen C, Bivard A, et al.; for INSPIRE. Bridging thrombolysis before endovascular therapy in stroke patients with faster core growth.
Neurology. 2023;100:e2083-e2092.



131. Campbell BC, Christensen S, Parsons MW, Churilov L, Desmond PM, Barber PA, et al.; EPITHET and DEFUSE Investigators. Advanced imaging improves prediction of hemorrhage after stroke thrombolysis.
Ann Neurol. 2013;73:510-519.



132. Campbell BC, Christensen S, Butcher KS, Gordon I, Parsons MW, Desmond PM, et al.; EPITHET Investigators. Regional very low cerebral blood volume predicts hemorrhagic transformation better than diffusion-weighted imaging volume and thresholded apparent diffusion coefficient in acute ischemic stroke.
Stroke. 2010;41:82-88.


133. Kim Y, Lee S, Abdelkhaleq R, Lopez-Rivera V, Navi B, Kamel H, et al. Utilization and availability of advanced imaging in patients with acute ischemic stroke.
Circ Cardiovasc Qual Outcomes. 2021;14:e006989.


134. Muir KW. Treatment of wake-up stroke: stick or TWIST?
Lancet Neurol. 2023;22:102-103.


135. Seners P, Yuen N, Mlynash M, Snyder SJ, Heit JJ, Lansberg MG, et al.; Mismatch Prevalence Investigators. Quantification of penumbral volume in association with time from stroke onset in acute ischemic stroke with large vessel occlusion.
JAMA Neurol. 2023;80:523-528.



136. El-Tawil S, Wardlaw J, Ford I, Mair G, Robinson T, Kalra L, et al. Penumbra and re-canalization acute computed tomography in ischemic stroke evaluation: PRACTISE study protocol.
Int J Stroke. 2017;12:671-678.



137. Mouridsen K, Thurner P, Zaharchuk G. Artificial intelligence applications in stroke.
Stroke. 2020;51:2573-2579.


138. Wardlaw JM, Mair G, von Kummer R, Williams MC, Li W, Storkey AJ, et al. Accuracy of automated computer-aided diagnosis for stroke imaging: A critical evaluation of current evidence.
Stroke. 2022;53:2393-2403.